F610
Orthopedic Problems
front limb | hind
limb | spine | skull | arthritis
| growing bone diseases | neoplasia
| fractures | infections
Introduction:
Orthopedics is the
branch of medicine and surgery that is concerned with the health of the bones
and associated tissues. There are many types of orthopedic problems that affect
dogs. It would actually be unusual for a dog to live its entire life-span
without experiencing lameness of one degree or another. Many of these incidents
are minor problems that can resolve on their own with rest and time. Minor
sprains, twists, or muscle bruises account for a large percentage of these
common problems. Persistent lameness, any lameness associated with trauma, and
severe lameness problems should always receive the attention of a veterinarian.
Recovery from an orthopedic problem may take weeks to months.
Many of the most common orthopedic problems in dogs are included in the
following information. Each disease or problem is categorized in this
information based on where it is located on the body. The front limb will be
covered first, followed by the hind limb. Diseases that affect more than one
area of the skeleton will then be covered separately.
Locating the problem area and potential cause:
Limping or lameness is one of the more common medical problems encountered by
dog owners. Often, the challenge comes when trying to determine the location and
then the cause for the lameness. At first, it is important to consider the
following questions. These are also questions that a local veterinarian may ask
when evaluating the animal:
- What is the activity level of the dog?
- Has there been any prior surgeries or medical problems?
- What is the animalís age, sex, breed, size, and diet? (For example,
young small breed dogs are more commonly affected by patellar luxation.
Osteochondritis dissecans, ununited anconeal process, fragmented coronoid
process, panosteitis, hypertrophic osteodystrophy, and hip dysplasia are
seen most often in immature dogs of large and giant breeds.)
- Is the dog currently on any pain or anti-inflammatory medications?
- Has the condition come on suddenly or slowly?
- Does the problem seem to be associated with an injury?
- Does the problem get worse after exercise?
A thorough physical and orthopedic examination should then be performed. The
goal of an orthopedic examination is to localize the cause(s) of lameness. The
following are some basic steps that are often used when performing an orthopedic
exam:
- The dog should be observed while standing. Signs of muscle shrinking
(atrophy), confirmation abnormalities, swelling, and pain can often be
found.
The normal dog will bear 60% of its weight on its front limbs. When severe
problems occur in the hind limbs, the dog will shift much of its weight to
the front limbs.
- Next, the dog is observed from the front, side, and rear while walking on
a leash and at a slow trot. When the lame limb contacts the ground, the
stride of the affected limb is usually shortened as compared to the
opposite, normal limb. When the sound limb hits the ground, the animal will
often spend more time with that limb in contact with the ground during the
walking motion. Other problems that are often noticed include ataxia (lack
of coordination), paralysis, paresis, and short, choppy gaits. If more than
one limb seems to have a problem, realize that a perfectly normal gait
requires the use of almost the entire nervous system and many of the muscles
and bones of the body. Injury, damage, or tumors that affect the nervous
system, muscles, or bones can cause problems in one, two, or all four limbs.
- Once the problem limb(s) is identified, a thorough examination of the
limb(s) is necessary to further localize the problem. The examination must
be systematic, starting at one end of the limb and proceeding up or down,
feeling every bone and every joint in the limb. Each area of the limb,
including muscles, bones and tendons, is felt (palpated) as gently as
possible until the painful area is identified. All this should be done while
the animal is fully awake without any sedation. Sedation may mask the animalís
response to the testing. Each joint is moved through the entire range of
motion by flexing, extending, and rotating. Each joint should also be felt
for evidence of swelling, pain, heat, lack of motion, instability, crepitus
(popping), and laxity.
Abnormal laxity (slackness) may indicate ligamentous injury or damage to the
joint capsule. Some fractures are often very obvious, while others may only
be identified by excessive movement of the area, pain, swelling, and lack of
use of the limb. A hot, swollen joint often is the result of an infection
causing inflammation. If the injury has caused the animal to not use the
limb(s) for a period of time, the muscles may shrink (atrophy). Injury to
muscles is often identified by tenderness, swelling, pain, and heat.
- After a specific area of injury has been identified, radiographs (x-rays)
are often used to help determine the extent of the damage and determine the
appropriate treatment.
Note:
Basic bone and muscle anatomy of
the dog can be found on page A34 of this manual. Pictures of actual radiographs
showing different orthopedic problems can be found at the end of this
information. The cost involved in treating an orthopedic problem may be
substantial. However, the outcome is often good to excellent with proper
treatment and patience.
Problems Found in the Front Limb:
Major orthopedic problems that commonly affect the front limb include
fractures, ligament and tendon injuries, growing bone diseases, dislocations,
infections, and cancers.
- Shoulder: The shoulder joint is the connection between the scapula
(shoulder blade) and the humerus (upper leg). Dislocations and fractures in
this area do occur but are unusual in dogs because the shoulder is
well-protected by surrounding muscles and other tissues. Arthritis (see
below) can also occur in the shoulder joint. Inflammation of a tendon
running through the joint and attaching to the biceps muscle is a rather
common source of pain in the shoulder. This is called "bicepital
tenosynovitis" and may occur because of excessive stress or other
shoulder conditions. Growing bone diseases, especially osteochondrosis (OCD)
(see below) are relatively common in the shoulder area. The shoulder is
also a common location for a deadly type of cancer called osteosarcoma (see
below).
- Bicepital tenosynovitis is a condition seen mainly in large breed
dogs. It can occur simply as a result of excessive exercise or working
stress on the shoulder, or it can be secondary to any other shoulder
condition. Exact diagnosis of this problem is usually not necessary but
may be obtained by x-ray studies with special dye injected into the joint.
Treatment consists of rest and the use of anti-inflammatory pain killers.
Surgery may be needed in the most severe cases.
- Shoulder joint dislocation can occur as a result of trauma in
dogs of any size or breed. X-rays are usually needed to tell the
difference between a shoulder dislocation and a fracture. Treatment always
requires professional help. Sometimes the dislocation may be successfully
treated by moving the bones back into place and wearing a special bandage
for 2 weeks. Often, however, surgery is a necessary part of the treatment.
Upper leg (humerus): The humerus is the long bone extending from the
shoulder to the elbow. Fractures of the humerus are common. The radial nerve
is one of the major nerves in the front limb and travels directly across the
surface of the humerus. This nerve can be damaged when the humerus is
fractured. Fractures of the humerus are easily diagnosed with x-rays and
always require surgery to repair (see figures #1 & #13).
 |
|
|
| Figure
1: Fractured Humerus - This is a fracture in the lower third of
the humerus. The black arrow indicates the lower portion of the
humerus that connects with the elbow. This type of fracture would
need to be repaired surgically. |
|
Elbow: The elbow joint is a "hinge" joint connecting the
humerus of the upper front limb to the radius and ulna of the lower front
limb. The elbow is relatively unprotected and can be easily damaged and
fractured. Dislocations of the elbow joint can also occur but seem to be less
common than fractures. Arthritis (see below) of the elbow joint occurs
commonly, especially in large breed dogs. A variety of growing bone diseases
affect the elbow joint. Some of these are discussed later. Osteochondrosis (OCD)
is a growing bone disease affecting many areas of the skeleton and is
discussed separately (see below). Bone and joint cancers can affect the
elbow joint but seem to do so with less frequency than in other locations in
the body.
- Fragmented medial coronoid process of the ulna (FMCP) is perhaps
the most common cause of pain in the elbow joint of young large breed
dogs. The ulna is a complex bone with several small projections at the
hinge area where it connects to the humerus. Most of these projections
develop separately in the young dog and attach themselves to their proper
locations on the ulna as the dog matures. The medial coronoid process is
one of these projections or attachments found on the inside surface of the
elbow. A developmental "accident" occurs in which the process
either attaches and then breaks off or fails to attach itself altogether.
This small piece of bone "floats" around in the elbow, causing
pain and inflammation. The fragment of bone is often too small to be seen
on normal x-rays and may require arthroscopy (camera-assisted surgery) to
diagnose. Treatment may be conservative, with anti-inflammatory pain
killers and regular, gradually increasing exercise. Surgery to remove the
fragment is also a possible treatment option. Arthritis is considered a
common consequence of FMCP and seems to occur regardless of treatment.
- Ununited anconeal process (UAP) is another growing bone condition
affecting the elbow. The ulna is a complex bone with several small
projections. The very top projection, which is part of the hinge mechanism
itself, is called the anconeal process. The anconeal process normally
grows separately from the main ulna bone in the very young dog, attaching
itself at about 4-5 months of age. If the process fails to attach itself,
it becomes a source of pain and inflammation in the joint. UAP was first
discovered in German shepherds and also occurs in Saint Bernards, Irish
wolfhounds, basset hounds, Labrador retrievers, dachshunds, Great Danes,
pointers, Newfoundlands, Great Pyrenees, weimaraners, and bloodhounds. UAP
is best diagnosed with x-rays (see figure #2). Surgery is considered the
best treatment option for most dogs, either by reattaching the process or
removing it altogether. Arthritis occurs later on in many cases but may be
lessened by early treatment. UAP is considered to have a genetic factor.
While the genetics controlling the passing of this condition on to the
next generation are complicated, it is recommended that any dog diagnosed
with UAP not be bred.
 |
|
|
| Figure
2: Ununited Anconeal Process - The white arrow identifies the
anconeal process that has been separated from the rest of the
ulna. See figure #14 below
for a picture of a normal elbow joint. |
|
- Elbow joint dislocation is uncommon but can occur as a result of
severe trauma. The joint is quite stable, and severe trauma is more likely
to result in a fractured bone than in a dislocation of the elbow. X-rays
are needed to tell the difference between fractures and dislocations of
this joint, and occasionally, both a fracture and dislocated elbow will be
seen together following a severe blow to a front leg.
Treatment of dislocations requires setting the bones in their proper
positions while the dog is under anesthesia. If the procedure can be done
within a few hours after the trauma, the setting of the bones can often be
performed without surgery. The more time that has passed since the
dislocation occurred, the more difficult it becomes to place the bones
back in their normal positions. Surgery is necessary to set the bones if
they cannot be replaced in their normal positions with anesthesia alone.
Placement of a splint or bandage after setting the bones in place may be
helpful to achieve rapid healing. Arthritis is common later in life in any
joint that has been dislocated.
Lower leg (radius/ulna): The radius and ulna are paired bones that
connect the elbow to the carpus or wrist joint. The radius is the major
weight-bearing bone of the two. Fractures of the radius and/or ulna are fairly
common in dogs (see figures #3 & #15). When fractures of the lower front limb occur,
both bones are usually broken together. However, it is not uncommon to have a
fractured radius and an intact ulna following trauma to a front limb. X-rays
are usually not needed to know whether a fracture of the lower front limb is
present but are important to determine the nature of the fracture (see
below). Many fractures require surgery, while others can be properly treated with
a cast or splint to stabilize the fractured bone(s).
 |
|
|
| Figure
3: Fractured Radius and Ulna: This is a transverse fracture of
both the radius and ulna. |
|
Carpus (wrist): The carpus is a very complex structure. There are
seven small bones in two rows that connect the lower front limb to the paw and
make up the carpal joints. There is a separate joint connecting each row of
bones, making a total of three joints in the carpus. Injuries to the carpal
joints and bones are common in dogs. Most of these are soft tissue injuries,
involving the ligaments and joint capsule only. X-rays are always needed
following injury to this area to examine the small bones of the carpus and to
determine if any fractures exist. Fractures can occur in any of the bones of
the carpus, although they are infrequent. Dislocations of the carpus can occur
along any of the joints. If there is severe damage to ligaments and other
structures that support the carpus, fusion of the joint (a surgical procedure
called arthrodesis) may be necessary. At least one condition related to
nutrition in puppies affects the carpus. The radius near its attachment to the
carpus is a very common site for a very serious type of cancer known as
osteosarcoma (see below).
- Hyperflexion deformity is a condition seen in puppies 6-12 weeks of
age. The Doberman pinscher breed is most commonly affected. The puppy stands
abnormally on both front legs, with the paws seeming to knuckle under.
Often, the condition improves on its own within a month or two. Exercise
should be restricted, and the puppy should not be fed any nutritional
supplements such as vitamin and mineral additives. Some studies show that
this condition may be a result of "overnutrition."
- Dislocation of the carpus can occur at any of the three joints as a
result of traumatic injury to the front limb. Damage to the ligaments and
other tissues that support the carpus is usually difficult to repair and
does not heal very well. Special x-ray pictures can help to diagnose a
dislocation at one or more of the three joints in the carpus. A dislocation
of any or all of these is generally termed "hyperextension." When
weight-bearing, a hyperextended carpus allows the paw to drop closer to the
ground than normal. The condition is usually quite painful. Minor cases of
hyperextension of the carpus may be successfully treated with a splint or
bandage and strict rest. However, most hyperextension situations require
more aggressive treatment. This is especially true among the medium to large
breed dogs. Fusion of the joint, a surgical procedure known as "arthrodesis,"
is necessary in many cases to restore function.
Paw: The canine front paw is made up of five digits (toes), four of
which are weight-bearing. The dewclaw, which corresponds to the human thumb,
sits high up on the inside surface of the front paw and does not bear weight.
There are five bones called metacarpals that extend from the carpus to each of
the five digits. Three bones make up each of the four weight-bearing digits.
These bones are called the first, second, and third phalanges. The dewclaw has
only two phalanges. The nail bed is a delicate tissue arising from the upper
surface of the last phalanx of each digit, and from this tissue each nail
grows. A thick, rubbery pad grows on the underside of each paw, and a smaller
pad grows on the underside of each of the digits. Lameness that results from
pain in the paw is common. Infections of the skin between the digits and
around the pads, abrasions of the pads themselves, and a variety of cuts and
scrapes all may result in pain and lameness. Fractures of the metacarpals and
the digits are also quite common. Finally, cancers of the paw usually arise
from the nail bed or the skin. Nail bed cancers can be extremely serious.
Problems Found in the Hind Limb:
Major orthopedic problem categories that commonly affect the hind limb
include fractures, ligament and tendon injuries, growing bone diseases,
dislocations, infections, and cancers.
- Pelvis: The pelvis is a bony structure responsible for
transferring the weight of the hind end to both hind legs. The pelvis is
divided into different areas. Weight is first transferred from the lower
spine to bones on the right and left sides. These bones are called the ilia
(singular = ilium). The ilia transfer weight to the hip joints. Connecting
the right and left sides of the pelvis are two other bone sets known as the
pubis and the ischium. The ilia, pubis, and ischium together make up the
pelvis, a box-like structure. The acetabulum is the socket-like portion of
the ilium that connects to the femur. See figures #16
& #17 for examples of a normal pelvis.
By far, the most common problem encountered involving the pelvis is trauma
and injury. Some estimations report that nearly 25% of all fractures involve
the pelvis. Other problems that may involve the pelvis include dislocations,
infections of the bone or surrounding tissues, and cancers.
- Pelvic fractures are extremely common with trauma of nearly
any type. Because of the rigid box-like shape of the pelvis, fractures are
always multiple and usually occur in sets of three (see figures #4 & #18). Pelvic
fractures range from minor to extremely devastating. Because the right and
left ilia are the main weight-supporting portions of the pelvis, fractures
of these bones are usually very serious. Fractures of the socket-like
acetabulum that houses the ball of the hip joint are also extremely
serious and usually end up causing arthritis of the hip later in life,
regardless of how well they heal. Fractures of the pubic bone are often
minor and are allowed to heal without intervention. Fractures of the
ischium vary in severity but are quite often allowed to heal on their own
because they usually do not affect the animalís ability to bear weight.
Diagnosis of pelvic fractures is made with x-rays. Treatment depends
completely on the situation. Many minor to moderate pelvic fractures can
heal very well with strict cage rest and anti-inflammatory pain killers
alone. More serious types of fractures, such as those that affect the hip
joint or cause changes in the natural shape of the pelvis, should be
treated with surgery. Surgery for pelvic fracture repair is extremely
difficult and is always expensive. Anti-inflammatory pain killers and
laxatives to help reduce pain of normal passage of bowel movements are
important aspects of the treatment plan for many pelvic fracture victims.
 |
|
|
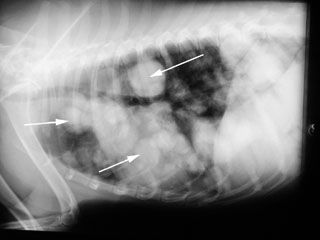
| Figure
4: Fractured Pelvis - Notice how the femurs and obturator
foramina (white arrows) do not line up. When the pelvis is
fractured, it usually breaks in at least three places.
See figures #16 & #17 for
examples of a normal pelvis. |
|
- Dislocations of the pelvis are also common with trauma. The only
place in the pelvis where a dislocation may occur is at the attachment of
the ilium to the spine. This is known as the "sacro-iliac
joint." A strong ligament that attaches the ilium to the spine may be
torn with severe trauma to the pelvis. Like pelvic fractures, pelvic
dislocations are diagnosed with x-rays and treated according to severity
and situation. Surgery is often the preferred type of treatment for pelvic
dislocations.
Hip: The hip joint consists of the "ball-and-socket"
structure connecting the pelvis to the hind limb. The femur is the first long
bone in the hind leg that connects the pelvis to the knee or stifle joint. The
femur is the longest bone in the body. As discussed previously, the medical
term for the socket is the acetabulum. The medical term for the ball is merely
the "head" of the femur. See figures #16
& #17 for examples of normal hips. A variety of conditions can affect the hip
joint. Fractures and dislocations are common. Arthritis of the hip joint can
be crippling to dogs and is discussed in detail later on. A strange condition
known as Perthesí disease affects the hips of young small breed dogs.
Cancers of the hip joint area do occur but are rare.
- Canine hip dysplasia is a well-known condition, especially
among owners of large and giant breed dogs. It has been diagnosed in small
and medium breeds as well. Dogs with hip dysplasia are born with normal
hip joints, but changes occur during development and aging. Gradual
loosening of the joint with swelling, pain, and damage to joint tissues
occurs. Months to years may pass, but the final result of hip dysplasia is
excruciating pain and crippling in the hind limbs.
There are three main contributing factors in hip dysplasia. The first and
probably most important of these is genetics. Because the condition is
passed on to future generations, any dog diagnosed with hip dysplasia
should not be bred. Screening programs for hip dysplasia in large or giant
breed dogs are extremely important and are considered standard procedure
for responsible dog breeders. X-rays are taken at two years of age or
older and sent to the Orthopedic Foundation for Animals (OFA). Expert
radiologists then study the x-rays and provide a score or category for the
dog. There are seven total possible scores, of which the top three are
considered normal. Most serious breeders will only consider a dog for a
breeding program if the result is "Excellent" or
"Good," the two top scores. People that purchase a large or
giant breed puppy should always ask about the OFA hip score for the
breeding parents.
The second factor that is known to contribute to hip dysplasia is diet and
nutrition. While less important than genetics in contributing to hip
dysplasia, this factor does make a difference and may be controlled by the
owners. While in the growing phase (birth to 12 months in most large to
giant breed dogs), it is recommended to feed a high-quality puppy formula.
Mineral/vitamin supplements are not necessary unless specifically
recommended by a veterinarian. Table scraps should be avoided. Treats
should be kept to a minimum, although used as needed for training
purposes. The high-quality puppy formula should be fed free-choice until
the puppy is four months of age. Starting at four months of age, it is
recommended to begin free-choice feeding at intervals. Usually, 30 minutes
twice daily is sufficient. This means that the puppy is offered as much as
it wants to eat for one half-hour every morning and again every evening.
This schedule should be followed until the dog is fully mature. Obviously,
adjustments may be necessary for each individual puppy. A puppy that eats
so much at the half-hour feedings that it becomes sick may require
free-choice feedings for only 10 minutes at a time, offered perhaps 3 or 4
times daily. At maturity, the dog should be switched to a high-quality
adult formula and fed a measured quantity based on its ideal weight and
the recommendations of the specific brand of food. Treats should still be
available on a restricted basis only. Over-nutrition and rapid growth in
puppies is an extremely common factor that can worsen the situation for an
animal prone to hip dysplasia.
The third known contributing factor for hip dysplasia is exercise and
activity level. Excessive exercise can lead to inflammation and loosening
in the young dogís joints and contribute to hip dysplasia, as well as
other problems. Moderate and controlled exercise is the key for any puppy
until it reaches maturity.
Diagnosis of hip dysplasia is made with x-rays. While a local veterinarian
may not provide an official OFA score for a dog, he or she can make a
diagnosis of hip dysplasia based on x-rays of the hip joints and the
pelvis (see figures #5, #19, #20, & #21). There are several options for treatment of hip
dysplasia. If diagnosed in a young dog, corrective surgery is available
that can help prevent the severe crippling arthritis that results. The
surgery is usually very expensive and requires a lengthy healing time.
Corrective surgery for older dogs consists generally in a total hip
replacement. This is a very difficult and expensive surgery that can have
miraculous results for a dog suffering from severe pain in the hips.
Medication such as cartilage protectants (glucosamine and/or chondroitin-containing
products) and anti-inflammatory pain killers are available, but these
drugs have a limited ability to prevent the pain and destruction in hip
dysplasia and will eventually fail in many cases. They are also very
expensive for large dogs and if used over a long period of time, will
likely cost a dog owner as much as surgery.
 |
|
|
| Figure
5: Hip Dysplasia - Notice that the head and neck of the femur
(white arrows) are irregular and enlarged. The head of the
femur has lost its smooth, round shape and does not fit nicely
in the hip socket (acetabulum). See figures
#16 & #17 for examples of normal hips. |
|
In summary, hip dysplasia is a challenging disease of the dog skeleton,
and treatment is usually expensive. It is best prevented through selective
breeding, proper nutrition, and avoiding excessive exercise. More
information on hip dysplasia is available under the heading
"Arthritis."
- Dislocation of the hip joint is another common result of injury
to the hind end in dogs. Blunt force trauma causes the ball to pop out of
the socket, tearing the ligaments and capsule that help keep the joint in
place. Diagnosis of this condition can often be made by examination by a
veterinarian. Confirmation of the dislocation is needed with an x-ray (see
figure #6). The x-ray is an important piece of information for proper
treatment because it will also show the veterinarian what type of
dislocation has occurred. Treatment consists of getting the hip joint back
together and keeping it there. This can be more challenging than it
sounds. If action is taken quickly, the head of the femur may be put back
into place by working the ball back into the socket. This is performed by
a veterinarian while the dog is under anesthesia. Because more
inflammation in the injured area actually "locks" the bones in
their abnormal positions, this procedure becomes increasingly more
difficult with the passage of time. If the dislocation cannot be repaired
in this manner, surgery becomes necessary to fix the problem. A variety of
methods are available, depending on the situation.
 |
|
|
| Figure
6: Dislocated Hip - The white arrow identifies the head of the
femur that is dislocated out of the hip socket (acetabulum).
Compare this side to the opposite hip that is not dislocated. |
|
A special bandage called an Ehmer sling is usually placed on the leg
regardless of the type of treatment used. This sling helps to keep the hip
in place while preventing the dog from putting any weight on the leg for
up to 2 weeks.
- Perthesí Disease (also known as "aseptic necrosis of the
femoral head"): This condition is not completely understood. It
appears that the blood supply to the head of the femur (the ball of the
ball-and-socket hip joint) is somehow damaged, leading to the death of
part of the bone. This leads to pain in the hip joint. Perthesí disease
usually affects only one hip. Breeds of dogs known to be affected by
Perthesí disease include Yorkshire terriers, West Highland white
terriers, dachshunds, Manchester terriers, Cairn terriers, miniature
pinschers, poodles, and Jack Russell terriers. Pain and lameness usually
start early, between 4 and 10 months of age. A veterinarian can diagnose
the condition with x-rays of the hip joints. Mild cases may be treated
with strict cage rest and anti-inflammatory pain killers; however, surgery
is generally necessary to free the animal from pain.
Upper leg (femur): The femur is the long bone extending from the hip
to the knee (stifle). Fractures of the femur are common. Fractures of the
femur are easily diagnosed with x-rays and always require surgery to repair
(see figures #7 & #22). Repair is often very difficult and can be very expensive.
 |
|
|
| Figure
7: Fractured Femur: This is a transverse fracture of the femur. To
adequately fix this type of fracture, orthopedic surgery is
required. |
|
Stifle (knee): The stifle joint is another hinge joint like the elbow
but vastly different in many ways. The lower portion of the femur ends at the
stifle joint. On the front side of the lower end of the femur sits the patella
(knee-cap), a small bone that moves up and down as the stifle bends. Small
cushions of cartilage sit in between the lower end of the femur and the upper
end of the tibia. These cushions of cartilage are called menisci (the lateral
meniscus on the outside and the medial meniscus on the inside). Two ligaments
run down the sides of the stifle joint, and two ligaments criss-cross inside
the stifle joint. All these parts are important in the function of the stifle
joint, and all can be injured and lead to pain and lameness.
Injury to the stifle joint is common, and may involve fractures, ligament
injuries, or dislocation. Probably the most common injury sustained to the
stifle joint is the tearing of one of the inner criss-cross ligaments. This
ligament is called the cranial cruciate ligament and is identical to the
anterior cruciate ligament in the human knee joint. Improper movement of the
patella or knee-cap (called patellar luxation) is also common. Arthritis of
the stifle is seen frequently in older patients, usually as a result of some
previous injury or problem in the joint. Growing bone diseases such as
osteochondrosis (see below) as well as bone cancers may also affect the
stifle area.
- Cranial cruciate ligament injuries occur very frequently in dogs
of all sizes and breeds. Large breeds of dogs are more at risk, however.
When the cranial cruciate ligament (CCL) tears, this allows the tibia to
slide forward away from the femur too much when the animal bears weight on
the leg. This excessive movement stretches the other tissues in the stifle
area, resulting in pain. The sliding movement also damages the cartilage
cushions (menisci) that sit between the two bones. Most dogs with a torn
CCL are very reluctant to bear any weight on the leg. The lameness is
usually sudden, although many dogs will have been exhibiting an on-off
mild lameness for weeks to months before. Tearing can happen in an
otherwise very healthy stifle joint with a sudden and severe blunt force
to the area. More commonly, however, the ligament will gradually weaken
and deteriorate as the animal ages. Aged, weak ligaments will often tear
easily with minor force, such as slipping or jumping. In many of these
cases, an owner will not know of any trauma received by the pet. It is
important to be aware that these ligaments age and become weak in both
stifle joints over time, and when the CCL tears on one side, there is a
good chance that the other will also tear in time. This likelihood is
probably made even greater with the extra weight borne by the
"good" leg when one ligament tears. Overweight dogs are more
likely to suffer CCL tears for the same reason.
Diagnosis of CCL tears is made during a detailed examination by a
veterinarian. The forward movement of the tibia is detected and helps
determine the diagnosis. Some dogs may need to be sedated for a thorough
examination if they are too tense. X-rays can also be helpful in showing
inflammation in the stifle joint but cannot show the actual torn ligament.
Torn cranial cruciate ligaments should always be repaired with surgery. If
not repaired surgically, the joint does stabilize itself the best it can
with thickening of tissues. The dog will improve gradually up to a limited
point after many months of lameness. However, arthritis will always result
and is often severe. Thus, if left alone and not repaired with surgery,
the dog will usually appear to improve for awhile but will end up getting
permanently worse in the end. Once the arthritis sets in, it is
irreversible. Prognosis with surgery is usually very good.
- Patellar luxation (dislocation of the knee-cap) is another very
common condition of the stifle joint of dogs. This condition occurs in
both small and large breed dogs, but the type of luxation is usually a
little different between the two. The patella usually dislocates towards
the inside of the leg (medially) in small breed dogs, while in large breed
dogs, it usually dislocates laterally (toward the outside). The small
breed version, known as medial patellar luxation (MPL), is more common.
Trauma to the stifle can cause dislocation in any type of otherwise
healthy dog. Patellar instability is graded based on its severity. Grade 1
is the most mild form, while Grade 4 is the most severe. The more mild
cases will often gradually progress to become severe later on. Many dogs
will adapt to the patella popping in and out of place as they walk. Some
dogs may hide this problem so well that the owner may not notice any
lameness until the problem is very severe. Arthritis of the stifle is
usually a consequence of patellar dislocation.
Diagnosis of this problem is made primarily by physical examination. A
veterinarian can detect the abnormal movement of the patella and determine
the severity of the problem. X-rays are helpful with the diagnosis,
especially in showing if any arthritis is present. Treatment depends on
the situation. Mild cases with no lameness present are monitored for
worsening of the condition. Severe cases require surgery. There is a large
gray zone in the middle of these two extremes. Treatment for cases falling
in this gray zone, with only occasional lameness and/or moderate
instability, must be judged individually by the owner and the
veterinarian. Surgery can be extremely helpful for one particular
individual but may not work at all in another. Small-breed medial (inside)
dislocation may respond very well to surgery, but success varies according
to the individual. Many cases of large-breed lateral (outside) dislocation
have other deformities as well and may not respond to any type of
treatment very well.
- Stifle dislocation is a very serious problem where numerous
ligaments and other tissues have been severely damaged. It requires a
great deal of force to cause dislocation of the stifle joint. Dislocation
of the stifle joint usually includes tearing and severe damage to both
cruciate ligaments and at least one of the menisci. Diagnosis is made by
careful examination by a veterinarian while the animal is under
anesthesia. X-rays are very helpful as well, showing damage to parts of
the joint that cannot be examined from the outside. Treatment is best
accomplished by carefully reconstructing the joint. Such a surgery may be
lengthy and very expensive. If reconstructive surgery is successful and
proper care is taken afterwards for healing, the outcome is often
surprisingly good. Mild arthritis and/or stiffness of the joint may
result.
Lower leg (tibia/fibula): The tibia and fibula are paired bones that
connect the stifle to the tarsus or ankle joint. The tibia is the major
weight-bearing bone of the two. Fractures of the tibia and/or fibula are
extremely common in dogs. When fractures of the lower hind limb occur, both
bones are usually broken together (see figure #8). However, it is not uncommon
to have a fractured tibia and an intact fibula following a hind limb trauma.
 |
|
|
| Figure
8: Fractured Tibia and Fibula - The view on the left is looking at
the leg from the side. The picture on the right is looking at the
leg from the front. This would be considered an oblique fracture. |
|
X-rays are usually not needed to know whether a fracture of the lower hind
limb is present but are important to determine the nature of the fracture (see
below). Treatment of certain cases requires surgery, while some
fractures may be properly treated with a cast or splint to stabilize the
fractured bone(s).
Tarsus (ankle): The tarsus or hock joint is a very complex structure.
There are seven small bones in two rows that connect the lower hind limb to
the paw and make up the tarsal joints. There is a separate joint connecting
each row of bones. The calcaneus (heel bone) is the largest of these bones and
projects back, toward the dogís tail. The Achilles tendon (common calcaneal
tendon) attaches to this bone and travels up to the muscles on the back of the
dogís lower limb. The Achilles tendon is rather exposed and can be injured
easily. Failure of the Achilles tendon also occurs due to fatigue. Injuries to
the hock joints and bones are common in dogs. Most of these are soft tissue
injuries, involving the ligaments and joint capsule only. X-rays are always
needed following injury to this area to help evaluate the small bones of the
hock and to determine if any fractures exist. Fractures can also occur in any
of the bones of the tarsus. Such fractures are uncommon, except in racing
greyhounds that commonly suffer fractures of the calcaneus (heel bone).
Dislocations of the tarsus can occur along any of the joints. If there is
severe damage to ligaments and other structures that support the tarsus,
fusion of the joint (a surgical procedure called arthrodesis) may be
necessary.
- Dislocation of the tarsus can occur at any of the joints as a
result of traumatic injury to the hind limb. Injuries to ligaments in the
joint and sometimes fractures of the small bones are associated with hock
dislocation. Diagnosis is made by careful examination by a veterinarian
and x-rays. Replacement of damaged ligaments, repair of fractured bones,
or fusion of the joint, also known as "arthrodesis," may be
necessary to restore function.
- Severing of the Achilles tendon is possible as a result of blunt
trauma or sharp injuries to the hind limb. Fatigue failure can occur as
well, resulting in swelling or even tearing of the tendon. Fatigue failure
is usually a result of gradual weakening of the tendon over months to
years. This type of injury is more common in dogs that are vertical
jumpers, such as Doberman pinschers and other breeds. Fatigue failure
results in a tendon that has lost its "spring" and provides
little support to the hock joint. Shortening of the tendon can be
accomplished with surgery. If the tendon has actually torn, surgery will
be necessary to repair it. Some cases respond to splinting or casting the
leg at its full stretched length, which helps the tendon to pull tight
again as it heals.
- Fractures of the calcaneus (heel bone) are common in racing
greyhounds but are infrequent among other breeds. This type of injury is
similar to the failure of the Achilles tendon but always requires surgery.
Paw: The canine hind paw is usually made up of four digits, all of
which are weight-bearing. The first digit, the dewclaw, which corresponds to
the human thumb, sits high up on the inside surface of the hind paw and does
not bear weight. The hind dewclaws are missing at birth in dogs more often
than they are present. Even when present, a large percentage of hind dewclaws
are attached to the paw by soft tissues only. The anatomy and problems
associated with the hind paw are identical to the front paw. See
above for information on the front paw.
Problems Found in the Spine:
The canine spine is divided into five sections. First, the cervical or neck
portion consists of seven vertebrae (bones that make up the spinal column). The
first cervical bone that connects to the base of the skull is called the atlas,
and the second cervical bone is called the axis. These two bones are distinct
from all other vertebrae in their shape. These bones, along with the other
vertebrae of the spine, provide protection for the delicate spinal cord that
runs through their center, while at the same time allow for some limited
movement in the neck and back. The second section of the canine spine is called
the thoracic spine and consists of 13 vertebrae. The 13 ribs connect on either
side of the chest to these vertebrae. The third section is called the lumbar
spine and consists of seven vertebrae that correspond to the "lower
back" in people. Three fused vertebrae make up the unique section of the
spine called the sacrum found in the pelvic part of the spine in dogs. The final
section of the spine is made up of a varying number of vertebrae that become
smaller and smaller as the tail tapers. These are called the coccygeal or tail
portion of the spine. Vertebrae have projections called processes that extend
dorsally (up) and laterally (sides). The processes are termed dorsal spinal
processes and lateral spinal processes. They vary in length and shape depending
upon where in the spinal column they are located. The dorsal spinal processes
are the small ridges that can be felt running the length of the back. These are
very useful in helping to count the vertebrae in the spine during examination.
Spinal column injuries can be devastating to an animal because any damage to
the delicate spinal cord running through the center of the spine can result in
permanent paralysis of portions of the body. Intervertebral disk disease, where
the cushion-like disks in between the bones of the spine become deformed, is
commonly seen in many breeds. Spinal injuries and diseases are more commonly
associated with the branch of medicine entitled neurology rather than with
orthopedics. A future update will concentrate on this topic.
Problems Found in the Skull:
The dog skull is extremely complex. It is made up of several bone plates that
fuse together as the dog matures, as well as the two paired mandibles or
jawbones with their hinges in the back of the lower skull. The central portion
of the skull houses the brain and brainstem that are critical to the function of
the entire body. Located in front of the brain and on the sides of the face near
the nose are open compartments known as sinuses. Hollow openings at the front of
the skull house the eyes. The paired mandibles from which the lower teeth grow
are connected to each other at the very front part of the skull by a strong
ligament and are hinged at the lower back portion of the skull by a joint known
as the temporomandibular joint (TMJ). The right and left maxillary bones make up
the sides of a dogís nose and are connected to each other on the bottom by the
palatine bone, hard palate, or roof of the mouth. The upper teeth grow from the
lower portion of the maxillary bones as it attaches to the hard palate.
Injuries to the skull occur relatively infrequently and are usually
associated with blunt trauma, such as an automobile accident. Fractures of any
bone in the skull can occur, and depending on what organs or soft tissues are
involved, these fractures can be very serious. Head trauma with severe brain or
brainstem injury is usually fatal. Most other injuries to the mouth, nose, and
face are treatable, although permanent disfigurement can result. Because the
possibilities of injury types are endless, each type of head injury must be
managed on an individual basis and under the care of a veterinarian.
Arthritis:
Arthritis simply means inflammation of a joint. Arthritis can be broken down
into several different categories based on the type, location, and cause of
joint inflammation.
Joints can be freely mobile, partially mobile, or immobile. While
inflammation can occur in any of these, the freely mobile joints and, to a
lesser extent, the partially mobile joints are those most likely to create
problems for the body when they do become inflamed.
The disk joints in between vertebrae in the spine are the most common
partially mobile joints where problems develop in the dog. Intervertebral disk
disease, where the cushion-like disks in between the bones of the spine become
deformed and cause back pain and sometimes paralysis, is commonly seen in many
breeds. Freely mobile joints include all the joints of the limbs such as the
shoulders, elbows, hips, stifles (knees), and all the joints in the paws
("knuckles"). While the specific makeup of each of these joints
differs, each contains the same basic structures.
A thin layer of cartilage overlying the bone in each joint provides for
frictionless motion. A thick, tough wall called the joint capsule attaches to
the bone on all sides and protects the delicate cartilage from damage. The joint
capsule also holds in the sticky, clear lubricating fluid that is found inside
the joint. This fluid is called synovial fluid and also helps with joint
lubrication and frictionless movement.
The three broad categories of arthritis seen in dogs include degenerative
arthritis (very common), infectious arthritis (uncommon), and immune-based
arthritis (uncommon).
- Degenerative joint disease (DJD) is the medical term for the
extremely common degenerative type of arthritis that occurs in joints.
Specific types of DJD have already been discussed, such as hip dysplasia (see
above). The main features of DJD are the wearing away of the
cartilage and the formation of new bone at the joint margins. Degeneration
of a joint can occur as a result of a long list of causes. As discussed in
the section on hip dysplasia, genetics, diet, and excessive exercise in a
growing puppy can be contributing factors. Previous injury to a joint or
nearby structures, infection, and age are also common reasons for this type
of arthritis to develop. DJD often gradually gets worse with time and may
become extremely severe and even crippling. Any freely mobile joint may
become affected, but in dogs the hips, elbows, and stifles are probably the
most likely to suffer from DJD. The most common reasons for these joints to
develop arthritis are listed in the specific sections for those joints. For
example, hip dysplasia is the most common reason for degenerative joint
disease in the hips, while tearing of ligaments in the stifle joint is very
often responsible for arthritis of that joint. Elbows become arthritic due
to a variety of causes, such as fragmented medial coronoid process and
ununited anconeal process (see above).
Clinical signs of this degenerative arthritis are generally limited to signs
of pain: limping, stiffness, reluctance to exercise, protectiveness and even
snapping when painful areas are touched. In severe cases, the patient may
stumble or fall frequently, may slip easily on stairs or slippery surfaces,
or may become unable to walk at all, if more than one limb is affected.
Because of the decrease in activity often associated with arthritis, dogs
may become overweight. This creates what is known as a "vicious
cycle," where the additional weight puts extra strain on the joints,
which makes the arthritis worse. This causes the dog to exercise or move
even less, leading back to more weight gain, and so on.
Diagnosis is based upon physical examination and x-ray films. Treatment for
degenerative joint disease is complex. Prevention is by far the most
effective way of dealing with any type of arthritis. One very good example
is the treatment for a torn cranial cruciate ligament in the stifle joint.
Without surgery, the chance of moderate to severe arthritis developing in
the joint approaches 100%. If surgery is performed soon after the ligament
has torn, however, arthritis will still probably develop but will likely be
mild. Once degenerative joint disease has developed for any reason,
prevention is not possible and other options must be considered. One
approach available for some types of arthritis is joint replacement surgery.
Joint replacement surgery is an extremely difficult and expensive treatment,
but it may offer the best possible result for some dogs. Total hip
replacement for hip dysplasia is available and may offer the best
alternative treatment. Other types of surgery may be helpful, such as joint
fusion or joint reconstruction. Decisions on whether surgery is an option
for treating joints already affected with DJD are best made with the help of
an orthopedic specialist.
Medical therapy for DJD is currently a very complex topic. Most dogs with
degenerative arthritis will benefit from medical therapy to some degree, and
in many cases the improvement is dramatic. Much of this improvement is due
to general pain relief. Another benefit of medical therapy is slowing down
the progression of disease. There are two main groups of medications that
are used to treat degenerative arthritis. The first group consists of
anti-inflammatory drugs that help reduce pain and restore function. The
second group consists of nutritional supplements containing natural hormones
and other products thought to protect the joint tissues from damage and even
change and improve the makeup of the joint tissues and fluid.
Many types of anti-inflammatory drugs have been used over the years in the
treatment of joint pain and arthritis in dogs. Anti-inflammatory drugs come
in two varieties: steroids and non-steroids. Non-steroidal anti-inflammatory
drugs are commonly known by the acronym NSAIDs. These include aspirin,
acetaminophen, ibuprofen, flunixin meglumine, phenylbutazone, ketoprofen,
pirixicam, etodolac, and carprofen. NSAIDs are becoming widely recognized as
an important part of the treatment of degenerative arthritis. As dogs become
arthritic, the pain of movement naturally leads to decreased exercise and
activity. Weight gain then becomes a common problem in less mobile pets.
Extra weight increases stress on the arthritic joints, leading to increased
inflammation and pain. The additional pain then causes the dog to become
even less mobile, and the "vicious cycle" mentioned previously
continues. Perhaps the greatest benefit of NSAID use in dogs with arthritis
is the breaking or hindering of this vicious cycle. Use of anti-inflammatory
pain killers can keep an arthritic dog moving and exercising, thus
maintaining a healthy weight and slowing down the progression of joint
disease.
Many different types of NSAIDs have been listed previously. This is not an
indication that all are recommended or healthy for use in dogs. In fact,
NSAIDs are drugs that tend to have a rather narrow margin of safety, which
means that it is quite easy to create problems with them. Side effects of
NSAID use include vomiting, listlessness, loose stools, and hives. It is
recommended to give NSAIDs to a dog only under the supervision of a
veterinarian and to use only those that have been specifically tested and
approved for dogs, such as etodolac (EtoGesic) and carprofen (Rimadyl - see
page G712).
Steroids can be used for their powerful anti-inflammatory effects in dogs,
but they are usually reserved for the most severe cases that fail to respond
to NSAIDs. Steroids are less likely to produce the long term benefits that
the NSAIDs can, mainly due to side effects such as weight gain.
A second major group under medical treatment of DJD is nutritional
supplement therapy. Glycosaminoglycans (GAGs) are substances naturally found
in joints and, specifically, cartilage. They are very important in
maintaining healthy joints. Several products are marketed with either the
actual glycosaminoglycan substance or the necessary building blocks the body
needs to produce them. Chondroitin sulfate is probably the most abundant and
commonly marketed GAG. It can be extracted from cow, whale, and shark
tissues. Glucosamine is an important building block for production of GAGs
in the body. It is commonly marketed along with chondroitin sulfate for
joint health in both people and animals. It is marketed under three major
types: glucosamine hydrochloride, glucosamine sulfate, and glucosamine
hydroiodide. All three appear to be equally effective. Some dog foods have
started marketing their products with added glucosamine and/or chondroitin.
It is thought by many nutritionists and veterinarians that these products do
make a difference if used over long periods of time. Studies in people have
found that these products do preserve motion in the joints and help control
joint pain. Glucosamine and chondroitin sulfate function in different ways
and appear to work best when given together. Some glycosaminoglycans may be
given as weekly or twice-weekly injections, but most are given as daily oral
tablets or powders. Another product that is commonly given is
methylsulfonylmethane (MSM). This is a naturally occurring dietary sulfur
that is a derivative of dimethyl sulfoxide (DMSO). It acts as an
anti-inflammatory and general pain reliever. Perhaps the major problem with
nutritional arthritis therapy is the lack of regulatory control over these
products. It is probable that the quality and quantity of the supplement
varies significantly from product to product. Most veterinary clinics sell
supplements that they feel contain a quality product for a reasonable price.
Examples of such products include Methylsulfonylmethane (MSM) (see page H506), Adequan (see page
H12), and Glyco-Flex III (see page H280).
- Infectious arthritis is the condition where an infection leads to
inflammation of a joint. There are several different types of organisms that
can infect the joints. Examples of bacterial infections, protozoal
infections, and fungal infections of joints will be discussed. Viral joint
infections occur in humans but are not known to occur in dogs at this time.
- Septic arthritis is the condition where a joint becomes infected
with bacteria, usually from a penetrating injury or bite wound. This
particular type of arthritis is discussed below.
- Lyme disease: Lyme disease is a type of infectious arthritis that
is caused by a specific bacteria called Borrelia burgdorferi. Borrelia
burgdorferi is spread by only one genus of tick, Ixodes, which
lives in specific areas. In the United States, Lyme disease is problematic
in the northeast states, north central states (northern Minnesota and
Wisconsin), and northern California/southern Oregon areas. Episodes of
lameness in one or more joints occurs typically, along with inflammation
and swelling of lymph nodes, lack of energy, and fever. Diagnosis is
sometimes difficult, but serology and culture of joint fluid may be
helpful. X-rays of affected joints may also be beneficial in some cases.
Antibiotics are used for treatment of Lyme disease and are usually quite
effective in a 3-4 week course. Products for tick prevention and
vaccination against Lyme disease itself can help prevent this type of
infectious arthritis. For more information on Lyme disease, see page F498.
- Mycoplasmal arthritis: Mycoplasma are small bacteria that
are difficult to culture and can sometimes be difficult to treat.
Fortunately, this type of bacterial arthritis is very uncommon. Mostly,
sick or debilitated dogs develop this type of arthritis secondary to a
respiratory or urinary tract infection. Diagnosis is made with special
tests performed on joint fluid. Treatment with antibiotics such as
erythromycin, tylosin, or gentamicin is usually recommended.
- Rocky Mountain spotted fever: This type of infectious arthritis
is caused by a bacteria-like microorganism known as Rickettsia
rickettsii that is spread by a tick. The genus of tick that carries
Rocky Mountain spotted fever is known as Dermacentor and is found
in the wooded areas of the central United States and eastern seaboard. The
disease is very serious and may result in sudden death. Walls of small
blood vessels are attacked and destroyed by the infection. This leads to
bruising and bleeding, death of tissues due to a lack of blood supply, and
inflammation of the eye, brain, and joints. Treatment with antibiotics
should be initiated as soon as possible following infection to minimize
the extent of disease. Tick control is very important in the prevention of
Rocky Mountain spotted fever. See F988
for additional details.
- Ehrlichiosis: Canine ehrlichiosis is another tick-borne disease
caused by a rickettsia. The brown dog tick, Rhipicephalus sanguineus,
is the tick species related to the spread of canine ehrlichiosis. The
infection causes damage to bone marrow and many other body systems.
Arthritis of several joints may occur early or late in the course of the
infection. Serology is usually used to diagnose this infection. Supportive
care and aggressive doses of antibiotics are the basic treatments for
canine ehrlichiosis. Tick control is probably the best method of
prevention.
- Leishmaniasis: Leishmaniasis is a disease caused by a protozoal
microorganism called Leishmania donovani. The sandfly serves as the
main insect carrier for Leishmaniasis. Areas where this disease occurs
include the Mediterranean, Africa, South America, and Asia. Most infected
dogs develop skin disease; lymph nodes, kidneys, eyes, and joints may
become inflamed as well. Diagnosis of Leishmaniasis is made with
laboratory testing of blood and swollen lymph node samples. Anti-protozoal
drugs do exist for Leishmaniasis treatment, but the most effective are not
available in all areas. Prevention is difficult in areas where
Leishmaniasis occurs. The best prevention advice for owners in non-endemic
areas is not to travel with their pets to endemic locations.
- Fungal arthritis: Fungal joint infections most often occur
secondary to fungal bone infections (see below under
"Infections"). A variety of fungal types may infect the joints
of dogs. Diagnosis is best made with special testing of the joint fluid. A
lengthy treatment with antifungal drugs is often necessary.
Immune-based arthritis is the third category of arthritis in dogs.
The term "immune-based" indicates that these types of arthritis
involve the animalís own immune system destroying the joint tissues.
Immune-based arthritis is typically a disease of multiple joints. This
category is split into two subsections titled erosive and nonerosive. Because
there is always destruction of the bone that borders the affected joint,
erosive-type arthritis is visible on an x-ray film. X-ray films of nonerosive
arthritis are essentially normal.
- Erosive immune-based arthritis:
- Rheumatoid arthritis is an uncommon type of arthritis in dogs where
the immune system forms antibodies against the joint tissues. These
antibodies then find joint tissues and stick to them, acting as a flag
to the rest of the immune system. Slowly, the tissues become swollen
and painful as the attack continues and the joints try to respond by
healing and protecting themselves from the immune system. Why the
antibodies form against joint tissues in the first place is not
completely known. However, distemper virus has been found in the joint
tissues of many dogs with rheumatoid arthritis, indicating a possible
link.
Any breed of dog may be afflicted with rheumatoid arthritis. Most
affected dogs are fully grown, and the average age when signs begin is
around 6 years. Lameness is the principal symptom noticed by dog
owners and can range from mild to severe. While multiple joints are
usually affected with rheumatism, the dog may experience pain in only
one or two joints. Sometimes, the lameness appears to shift from one
joint to another. Joints may become swollen and deformed in time.
Diagnosis of rheumatoid arthritis is somewhat complex, generally
requiring x-ray films, joint fluid analysis, and blood testing.
Similar to people, rheumatoid arthritis is not curable and is
generally treated with a variety of anti-inflammatory drugs. NSAIDs,
steroids, gold injections, and other types of therapy have been
attempted with some success. Limited response has been seen with some
types of surgery. Rest and elimination of stress are important in
treatment of rheumatoid arthritis.
- Greyhound polyarthritis is an erosive immune-based arthritis seen
only in the greyhound. Most affected dogs gradually become lame before
age 3. This type of arthritis appears similar to rheumatoid arthritis,
but there is evidence that Mycoplasma bacteria (see
above) may be responsible and that this type of arthritis should be
categorized as an infection. Diagnosis and treatment of greyhound
polyarthritis are similar to rheumatoid arthritis.
- Nonerosive immune-based arthritis:
- Systemic lupus erythematosus (SLE) is an uncommon disease in dogs
that affects multiple systems in the body at one time. Disorders of
the nervous system, respiratory system, kidneys, skin, muscle tissue,
blood, and joints are commonly seen with SLE. Multiple joints
typically become swollen and painful. Affected animals may be
listless, have a decreased appetite, and may have a high temperature.
If the kidneys begin to fail, an increased thirst and need for
urination may develop. Skin problems are common and are described in
more detail on F770. Because SLE tends to involve so many
systems, diagnosis of this disease is challenging. Tests that may be
helpful in the diagnosis of SLE include testing for antibodies the
immune system creates to attack other tissues of the body, also known
as "autoantibodies;" x-ray films, joint fluid tests, and
bloodwork. Treatment is generally focused on suppressing the immune
system with steroids and other drugs. The expected outcome is not
usually good and becomes very grim if the kidneys begin to fail.
- Breed-specific polyarthritis: This is a group of uncommon to rare
conditions specifically seen in certain dog breeds where the immune
system is responsible for swelling and pain in the joints and
sometimes in other parts of the body as well. Most of these conditions
are difficult to treat and carry a rather poor prognosis. These
include the following:
- Polyarthritis/polymyositis syndrome: Seen most often in spaniel
breeds. Inflammation occurs in joints and muscle tissue.
- Polyarthritis/meningitis syndrome: Seen in weimaraners,
pointers, boxers, Akitas, and Bernese mountain dogs. Inflammation
occurs in joints and the meninges (tissue lining the brain and
spinal cord). Severe neck pain and difficulty walking may be seen.
- Familial renal amyloidosis: Also known as the "hot hock
syndrome," this is a disease found in Chinese shar peis. Hock
joints become inflamed, swollen, and painful. Failure of other
organs, especially kidneys, usually results in a very poor
outcome.
- Heritable polyarthritis of the adolescent Akita: As described in
the name, young Akitas are affected. Inflammation of joints, lymph
nodes, and other organs may occur.
- Polyarteritis nodosa: This uncommon condition may be seen in a
variety of breeds and is often called "stiff beagle
disease" when it occurs in young beagles. Joints, meninges
(protective tissue around the brain and spinal cord), and muscles
may become inflamed. Severe neck pain is often present if the
meninges are involved. Because it can gradually go away on its
own, this condition may have a good outcome when it occurs in
young dogs.
- Idiopathic polyarthritis is a "catch-all" category where
all other unknown causes of multiple joint pain and swelling are
placed. About half of the arthritis cases placed into this category
appear to result from illness elsewhere in the body. Three types of
illness located in other parts of the body can lead to this type of
arthritis, although it is usually unclear how this happens. First,
infections in various places including the lungs, tonsils, urinary
tract, skin, and eyes have been linked with idiopathic polyarthritis.
Disease of the digestive tract including inflammation of the stomach,
intestines, and colon is another cause of idiopathic polyarthritis.
The third cause is cancer of remote areas including breast cancers and
some types of cancer involving the heart, reproductive tract, and
skin. If arthritis of several joints occurs due to any of these
underlying conditions, the treatment must focus on the specific
condition. If an underlying cause can be treated and removed, the
arthritis will usually go away. The other half of cases diagnosed with
idiopathic polyarthritis do not have any known underlying cause for
the problem. Most of these cases respond well to treatment with
steroid therapy.
Growing Bone Diseases:
- Osteochondrosis: Osteochondrosis (OCD) is a common disease of
growing dogs. Large breed dogs are most likely to suffer from OCD,
especially the golden and Labrador retriever, rottweiler, Great Dane, Saint
Bernard, German shepherd, and boxer. Males are more likely to be affected
than females. Lameness generally becomes apparent between 4 and 12 months of
age.
To fully understand the disease, the following brief discussion of how bones
grow is necessary. Growth plates are thin lines of new bone growth and are
found near the ends of all long bones and at other various locations
throughout the skeleton. Each bone is formed by growth starting from these
growth plates. Growth plates can be seen on x-rays and even leave scars that
can still be seen in the bones of fully mature animals. A trained
professional knows where growth plates belong in each bone and is able to
look at x-rays to determine if a specific line through a bone is normal or
abnormal. Bone growing from these growth plates begins as cartilage cells
that gradually turn into bone cells. Osteochondrosis (OCD) is a disease
describing the failure of a group of cartilage cells to fully turn
themselves into bone cells. Even partially changed cartilage does not act as
true bone and may cause problems.
As the abnormal portion of undeveloped bone is pushed out to the surface of
the joint by continuing growth from underneath, pain often results. The
portion of abnormal tissue is weak and easily broken off the surface below
it. Sometimes, a flap is created that is attached at one side but not the
other, while in other cases the entire portion of hard abnormal tissue
breaks free and floats around in the joint space. Ostochondritis dissecans
is the medical term used to describe a detached flap of tissue in the joint.
In any of these situations, inflammation occurs inside the joint and causes
pain to the dog, resulting in lameness.
Several factors have been identified that may lead to OCD in dogs. First,
genetics do play a role, but the extent of inheritance from one generation
to another is unclear. Second, trauma to a joint is suspected to lead to OCD
in some dogs, and this is particularly under suspicion in the elbow joint.
Fragmented medial coronoid process (FMCP) (see above) in dogs is
probably related to OCD of the elbow. Third, a higher incidence of OCD has
been seen with overfeeding large breed puppies. Nutritional factors are
thought to be the cause, especially over-supplementation of calcium. A lack
of vitamin C has also been tied to OCD lesions. Finally, certain toxic
substances are known to cause OCD, such as those produced by some fungi.
This type of OCD is very unlikely to occur in the general dog population.
There are at least 35 known areas in the skeleton where OCD can occur.
However, in the dog skeleton, four main joints are affected. The shoulder
joint is the most common of these. Other joints commonly affected include
the elbow, the stifle, and the hock joints.
Diagnosis of OCD is based on physical examination by a veterinarian and
x-rays (see figure #9). Sometimes, special x-rays where dye is injected into
the affected joint may be needed. The dye can travel underneath a small flap
of abnormal tissue and make it much more visible than it would have been
otherwise. Treatment of OCD depends on the individual situation. Some mild
cases of shoulder OCD in very young dogs, for example, may be successfully
treated with strict rest only. At one time, it was recommended to force the
dog to exercise until the flap of abnormal tissue broke free. The theory was
that once free, the tissue would be absorbed and the problem solved.
However, it has been shown that the free floating piece of tissue is
nourished by the joint fluid and may actually grow instead. Therefore, this
treatment plan is no longer recommended. Nutritional therapy, especially
vitamin C supplementation, may be advised by some veterinarians. However,
some controversy does occur among professionals concerning giving large
quantities of vitamin C. Probably of more importance is ensuring that the
growing large-breed puppy is not overfed. Surgical treatment of OCD is the
most common approach and consists of removing all abnormal tissue from the
affected joint. As with most types of orthopedic surgery, OCD flap removal
is often expensive. However, the outcome is usually very good, with minimal
joint disease resulting later in life.
 |
|
|
| Figure
9: Osteochondrosis - The black arrow identifies an area (dark
spot) of osteochondrosis in the head of the humerus. The
shoulder joint is a common place for osteochondrosis. |
|
- Panosteitis is considered a growing bone disease because it most
typically affects growing puppies of the large breeds, especially German
shepherds. Panosteitis is an inflammation of the long bones causing pain and
lameness in young dogs 6-18 months of age. Many possible causes have been
suggested, but none has been proven. An affected dog will have periodic
lameness lasting 1-3 months at a time. The lameness may move from one leg to
another in the course of the disease. Long bones of both the front and hind
limbs are affected. Affected dogs may also have a fever, lack of energy, and
experience weight loss. In most cases, diagnosis may be made with x-rays.
The disease is "self-limiting," meaning that it goes away on its
own in time. Therefore, treatment is not necessary, but most affected dogs
will benefit from anti-inflammatory pain killers until the condition is
gone.
- Hypertrophic Osteodystrophy: Hypertrophic osteodystrophy is another
growing bone disease where puppies, usually of the large breeds, experience
lameness between the ages of 2 and 8 months. Pain and swelling near the ends
of the long bones (specifically affecting a region of the bone called the
"metaphysis") are often seen with this condition. Sometimes, the
puppy may have a fever, lack of appetite, and experience lethargy.
The most common region for this condition to affect is the lower front leg,
just above the carpus (wrist) joint. It can, however, affect either end of
any of the long bones. The cause of hypertrophic osteodystrophy is not
known, but nutritional problems have been suggested. Vitamin C deficiency is
probably the most well-known suspected nutritional cause, but this has not
been proven. However, treatment with vitamin C is still often recommended.
Diagnosis is made with physical examination by a veterinarian and x-rays
(see figure #10). Treatment is supportive only at this point. Making sure
the pet has adequate fluids and a well-balanced diet (but not overfed!) are
important. Anti-inflammatory pain killers are frequently used to help give
the animal some comfort. Outcome is usually very good, with a complete
recovery. The most severe cases, however, may not recover at all, and some
pets have been euthanized for this condition.
 |
|
|
| Figure
10: Hypertrophic Osteodystrophy - The black arrow identifies an
area of hypertrophic osteodystrophy just above the growth plate
of the radius. The area can be identified by its dark (radiolucent)
appearance. |
|
Neoplasia:
Neoplasia or cancer is a common orthopedic disease. Orthopedic cancers are
broken down into primary cancers (originate in the bone) and secondary cancers
(spread to bone from somewhere else).
- Primary bone cancers: Osteosarcoma, chondrosarcoma, fibrosarcoma,
and hemangiosarcoma are the four most prevalent primary bone cancers seen in
dogs. Osteosarcoma is by far the most common.
- Osteosarcoma is the most common bone cancer in dogs and arises
from bone cells. This type of bone cancer is extremely aggressive and
usually spreads very quickly to other parts of the body. Most at risk are
large and giant breeds such as the St. Bernard, Great Dane, Irish setter,
Doberman pinscher, boxer, and German shepherd. Middle-aged to older dogs
tend to be affected most often, although osteosarcoma has been seen in a 6
month old puppy. Osteosarcoma can arise from any bone of the skeleton.
About 80% of this type of bone cancer occurs in the long bones of the
limbs. The other 20% can occur in the skull, spine, ribs, and other bones.
In the limbs, the most common places where osteosarcoma occurs are the
shoulder (upper humerus), carpus (lower radius), and knee (both lower
femur and upper tibia).
The cause of osteosarcoma in dogs is unknown in most cases. A higher risk
does seem to be associated with any abnormal bone (i.e. affected by
another bone disease), places where a fracture occurred in the past, and
with metal hardware, such as screws or pins in a previously broken bone.
Radiation may also be a cause of bone cancer. However, since most dogs
affected with bone cancer do not fit into any of these possible
categories, it is usually impossible to give a reason for its occurrence.
The most obvious clinical signs of osteosarcoma include pain and swelling
in the affected area. When the bone cancer occurs in one of the limbs,
lameness is often very obvious early on. Depending on where the cancer
occurs, swelling of the affected area may become obvious to an owner.
Another clinical sign may occur where the cancer, after weakening the bone
from which it grows, allows the bone to break through the weakened area.
This is known as a pathologic fractureĖ a fracture of a bone resulting
from some underlying cause. When such a fracture occurs, sudden lameness,
inability to bear weight, pain, and swelling at the fractured area result.
Diagnosis of osteosarcoma begins with x-rays of the affected bone. Trained
professionals can come to a very high degree of suspicion for osteosarcoma
just by looking at a good quality x-ray (see figure #11). For a complete
diagnosis to be made, a biopsy of the cancerous tissue must be sent to a
laboratory for histopathology. A bone biopsy is a tricky procedure with
the undesirable side effect of further weakening the diseased bone.
Treatment for osteosarcoma is so aggressive and drastic, however, that an
accurate diagnosis is very important. The benefits of knowing the
diagnosis outweigh the risks of obtaining a bone biopsy in most cases.
Once the diagnosis of osteosarcoma is made, treatment should be started as
soon as possible. Treatment of osteosarcoma begins with aggressive removal
of the affected bone. Amputation of the entire affected limb is the
standard approach for osteosarcoma of the long bones of the legs. For
osteosarcoma of a rib, surgery can be performed to remove the cancerous
tissue and replace the rib with a special mesh or other supportive
material. Complete removal of skull or spinal osteosarcoma may be
extremely difficult to impossible depending on how extensive the tumor has
spread.
 |
|
|
| Figure
11: Osteosarcoma: The white arrow identifies the center of an
osteosarcoma tumor in the top section of the humerus. |
|
A rather recent alternative to amputation can be offered for some
patients. This technique, known as limb-sparing surgery, was developed to
save the affected limb from amputation. The cancerous portion of the bone
is removed and replaced with a section of healthy donor bone from another
dog. The donor bone is secured with a metal plate to the original bone.
This surgery is very expensive but an attractive alternative for some
owners not wishing to have their petís limb amputated. The technique
does not appear to affect the survival rate of dogs when compared with
amputation. Most often the technique has been used with osteosarcoma near
the carpus (lower radius). Shoulder (upper humerus) osteosarcoma may also
be treated in this way, but recovery from surgery usually takes longer.
Osteosarcoma of the hind limb is usually not treated with limb-sparing
surgery.
Most of the time, the cancer has already spread to the lungs (see
figure #23 below) by the time
the diagnosis is made. Chemotherapy can help slow the growth of the cancer
wherever it has spread for months to sometimes years. A veterinarian
specializing in cancer treatment may make the best recommendation on
chemotherapy based on the most current information available. Prognosis
without treatment of any kind is poor, with the pain increasing in
intensity very quickly. Amputation alone for osteosarcoma of a limb can
provide wonderful relief from pain to a pet, but without additional
treatment (i.e. chemotherapy) survival rates for these animals is usually
only 4 or 5 months. With amputation and chemotherapy, months to years may
be added to the life of a pet. The sad news is that eventually nearly all
patients diagnosed with osteosarcoma will die from the disease sooner or
later.
- Chondrosarcoma is a primary bone cancer that arises from
cartilage cells within the bone. It is far less common in the limbs than
osteosarcoma but does occur with some frequency in the ribs and skull. It
can occur in any area of the skeleton. This type of bone cancer is very
aggressive but has a lower rate of spreading to other areas in the body
than does osteosarcoma; this is another reason why it is important to make
a complete diagnosis based on bone biopsy. Diagnosis consists of x-rays
followed by biopsy of the affected bone. Treatment consists of aggressive
surgical removal. Radiation therapy has been used in chondrosarcoma
therapy, but success has been variable. Currently, chemotherapy is
probably the least useful cancer treatment for chondrosarcoma.
- Fibrosarcoma is a cancer arising from connective tissue found
throughout the body, including bone tissue. It occurs only rarely in bone
but may be difficult to treat. Diagnosis is made by bone biopsy.
Fibrosarcoma of bone, in contrast to other tissues, is more likely to
spread to other areas of the body and cause further disease and even
death. Aggressive surgery is considered the best treatment.
- Hemangiosarcoma is a cancer of blood vessel cells that rarely
occurs in bone. When it does occur in bone, spreading to other tissues is
very common and the affected dog most often suffers from secondary
spreading to brain, lungs, liver, and other organs.
Primary joint cancers:
- Synovial sarcoma is an uncommon cancer arising from cells in and
around the joints. In dogs, synovial sarcomas seem to affect the knee
joint most frequently, followed by the elbow joint. Lameness is the most
common sign noted with this cancer type. The average age of affected dogs
is 7-8 years old.
Diagnosis is made with x-rays and biopsy. Amputation of the affected leg
is standard treatment for synovial sarcoma, with the possibility of
chemotherapy. The outcome is good to fair with amputation of the affected
leg, and some cases may go up to 2 years without recurrence.
Secondary bone cancers: Tumors that spread from other areas of the
body to bone are called secondary bone cancers. Spreading can occur through
the blood supply to bone from distant places in the body or from tumors that
grow right next to the bone and invade it. Most commonly, secondary cancers
occur in bone from nearby tumors that invade and attack all tissues nearby.
Many cancers that start in the mouth and in the toes (especially the nail bed
tissue) are especially prone to invade bone. Distant spreading can occur from
cancer of the lungs, liver, thyroid gland, prostate gland, and mammary gland
(breast cancer). Sometimes the source of the cancer is not known until a
biopsy is obtained of the affected bone and a veterinary specialist finds, for
example, cancerous thyroid gland cells within the bone. Treatment of spreading
secondary bone cancer depends on the nature of the cancer. Treatment of the
original tumor is usually of more importance than treatment of the secondary
bone cancer. Surgery, chemotherapy, or radiation therapy may be feasible
treatment options.
Fractures:
Broken bones are perhaps the most common orthopedic problem encountered in
dogs. Falls, gunshot injuries, and automobile accidents are all common causes of
broken bones in pets. This section will address the basics of dealing with
fractured bones in a practical sense for dog owners.
- Classification of fractures:
- Closed or simple fracture: This is a fracture of a bone where
the skin is not broken and no communication to the outside environment
has occurred. It is opposite of an open or compound fracture.
- Open or compound fracture: This is a fracture where
communication with the outside environment has occurred. Examples
include gunshot injuries to bones and fractures where the sharp bone
fragments have cut through the skin.
- Transverse fracture: This is a fracture where the bone is
broken into two pieces and the fracture crosses the bone in a straight,
side-to-side line.
- Oblique fracture: This is a fracture where the bone is broken
into two pieces and the fracture crosses the bone in a diagonal line.
- Spiral fracture: This is a fracture where the bone is twisted
apart.
- Comminuted fracture: This is a fracture where the bone is
broken into multiple pieces.
- Greenstick fracture: This is a fracture where the bone is
broken on one side, with the other side bent but not fractured. This
type of fracture is most commonly seen in young puppies.
- Pathologic fracture: This is a fracture due to a weakened bone
structure from any disease process (i.e. bone cancer, infection, or
osteoporosis).
- Stress fracture: This fracture results from repeated force to a
bone. This type of fracture is most commonly seen in performance dogs.
- Segmented or double fracture: This is a bone that is
broken in two or more different places.
Managing fractured bones: The first part of treatment of a broken
bone is often done by the dogís owner. Since most fractures are associated
with some kind of trauma, checking the vital functions of the injured pet
should always be done first. Alertness, breathing status, and mucous membrane
color/capillary refill time should be observed quickly and thoroughly. The petís
responsiveness and state of awareness can help assess whether the brain and
central nervous system are functioning on a basic level. Difficulty breathing
may result from internal bleeding, broken ribs, or other injuries. Pale gum
color with a slow capillary refill time occur with severe blood loss and
shock. These are potential life-threatening injuries that must take precedence
over any broken bones. Rapid transport to a veterinary hospital is very
important for trauma patients. Specific home treatment for a broken bone can
be done if there is time and if the patient is cooperative. Handling an
injured pet should always be done with cautionĖ even the most trustworthy
pet may bite its owner when injured. If a wound is present in association with
a broken bone, a clean bandage may be placed on the injury. Direct pressure
should be used to control any bleeding from an injured limb. See page E200 for
additional emergency treatment information.
Once the patient is brought into the veterinary hospital, the veterinary staff
takes over, repeating the steps listed above. Beginning with the vital signs,
the patient is examined thoroughly. Life-threatening injuries are given
attention first, followed by fractured bones. A patient must be stabilized
before a broken bone is given treatment; this stabilization process may
require hours to days. A bandage is usually placed on a fracture to help
control pain and prevent further injury until proper treatment can begin. Once
the patient is stable, plans for treating broken bones may be made.
Specific treatment for a broken bone depends greatly upon the situation. The
location and type of fracture, availability of specialist help, nature of the
patient, and cost are all factors that influence how a broken bone will be
treated. Some veterinarians specialize in orthopedic surgery and should become
involved in the more complex bone injuries. Because they usually require a
great deal of time, personnel, and training to properly treat, the cost of
treating broken bones is generally high.
There are various methods of fixing broken bones. The broken bone must be
placed into the proper position and held there with some type of supporting
device. Splints and casts are rigid supports that encircle the broken limb and
can be used for a variety of fractures, but have limitations on how much they
can do. These types of outer support can be used with or without internal
support for the broken bone, depending upon the situation. Other types of
support for broken bones may require extensive surgery. Metal pins inserted
into the bone (see figure #12), wires that encircle the fracture and tighten
against the outside of the bone, and metal plates that cross a fracture and
are screwed into the bone are all common types of internal support that are
used. External skeletal fixation is another type of support that is becoming
more common in veterinary medicine. This type of support is both internal and
external because several metal pins are drilled at a right angles to the bone
with the pin sticking out of one and sometimes both sides of the leg. These
pins are then connected to each other with another metal rod or bone cement,
creating a support on the outside of the body. The type of support used to
treat any given fracture depends upon many factors and is best left to the
discretion of the veterinarian.
 |
|
|
| Figure
12: Osteomyelitis - The black arrows identify just one area of
osteomyelitis surrounding the humerus. The white arrow identifies
a bone pin placed to repair a previous fracture. |
|
Infections:
Infections of bones and joints can occur in dogs. Infection of bone tissue is
called "osteomyelitis" and infection of a joint is called "septic
arthritis."
- Osteomyelitis is the medical term for bone infections. Bone
infections may involve bacteria, fungi, or viruses. Bacteria are responsible
for most bone infections seen in dogs. Any dog may be affected, and any part
of the skeleton may become infected. Bone is typically well-protected and
resistant to infection. Open fractures (see above), where the broken
ends of the bone penetrate the skin, are perhaps the most common way the
infection arrives at the bone. Infections may also enter bone tissue
following surgery, from infected wounds near the bone, or from the blood
supply. Chronic long-term bone infections can result from open fractures and
bone surgery. If a fragment of bone dies and is left in the fracture area,
new bone may form around it and trap it inside the healed bone. The immune
system cannot fight infection inside of dead tissue since it is cut off from
the bodyís blood supply. Thus the trapped piece of dead bone provides an
excellent home for bacteria and leads to long-term infection. Diagnosis of
osteomyelitis is usually made with a good history, physical examination, and
x-rays (see figure #12). Treatment of osteomyelitis depends upon the
situation. Antibiotics and surgery are the primary means of treating
bacterial bone infections. Surgery is needed in most cases of long-term
osteomyelitis to remove pieces of dead and severely scarred tissue.
Antibiotics are provided for several weeks to months.
Coccidioidomycosis is a fungal disease caused by Coccidioides immitis that
occurs in the southwestern United States. This fungus is inhaled by the dog.
In about half of the infected dogs, many systems of the body, including the
skeletal system, can be involved. Diagnosis may be made by blood testing and
special skin reaction tests. X-rays show bone infection that may appear
remarkably like bone cancer. Biopsy of bone may be needed to provide an
accurate diagnosis. Treatment with anti-fungal drugs such as ketoconazole
and amphotericin B is warranted, but the outcome may be poor even with
treatment. Other types of fungi that may infect bone, although less
frequently than Coccidioides immitis, include Blastomyces
dermatitidis, Histoplasma capsulatum, and Cryptococcus
neoformans.
- Septic arthritis is the term used for an infected joint. Injuries
to joints are the most common reason for infection to reach these
well-protected areas. Other sources of infection into joints include
injections directly into a joint, surgery, and access through the blood
supply. The dog is usually in pain, reluctant to bear weight, and may have a
fever. The joint may be hot and swollen. Diagnosis of a septic joint is
achieved by history, physical examination, x-rays, and by testing a sample
of the joint fluid. The joint fluid test is the most helpful of the tests in
showing the actual infection. Culture and sensitivity (see page D135) may be
performed on the fluid, often providing very helpful information for
treatment. Septic arthritis is a difficult problem to treat. There is
usually extensive and permanent damage done to the delicate tissues of the
joint, which results in permanent pain and arthritis even after the
infection is gone. Surgery to relieve swelling and pressure, flushing the
joint with sterilized fluid, and removing any clumps of infected material is
usually the best approach. Sometimes, the joint must be left open and
carefully bandaged to allow it to drain. Administration of antibiotics for
at least 4 weeks is very important regardless of the surgical approach. The
outcome is very questionable, and permanent damage resulting in arthritis of
the joint is not uncommon.
Summary: Orthopedic problems are a common occurrence in veterinary
medicine. The key to successfully treating these problems is early detection and
proper treatment. The petís owner plays an essential part in identifying
problems early and then seeking the proper medical attention. In general, if
lameness in a pet lasts longer than 24 hours, the lameness is getting worse, or
there is an obvious injury, veterinary advice should be sought.
The following pictures are radiographs that represent some of the common
orthopedic problems encountered in veterinary medicine. Some are similar
to the radiographs shown previously, while others are pictures of normal joints
and bones.
 |
|
|
| Figure
13: Fractured Humerus - This is a fracture in the lower third of
the humerus. |
|
 |
|
|
| Figure
14: This is a completely normal elbow joint. |
|
 |
|
|
| Figure
15: Fractured Radius and Ulna: This is a transverse fracture of
both the radius and ulna. |
|
 |
|
|
|
Figure
16: This is a completely normal pelvis. The hip sockets and head
of each femur are also normal. Notice the smooth, rounded head of each
femur and how they fit nicely into each hip socket (acetabulum).
|
|
 |
|
|
| Figure
17: This is also a completely normal pelvis. The hip sockets and head
of each femur are also normal.
|
|
 |
|
|
| Figure
18: Fractured Pelvis - Notice how the obturator foramen (white arrow) is
not a smooth "circle." When the pelvis is
fractured, it usually breaks in at least three places. |
|
 |
|
|
| Figure
19: Hip Dysplasia - Notice that the head and neck of the femur
(white arrows) are irregular and enlarged. The head of the
femur has lost its smooth, round shape and does not fit nicely
in the hip socket (acetabulum). |
|
 |
|
|
| Figure
20: Another picture of hip dysplasia - The neck of each femur (white
arrows) is severely thickened. |
|
 |
|
|
| Figure
21: Another picture of hip dysplasia. |
|
 |
|
|
|
Figure 22: A severely fractured femur.
|
|
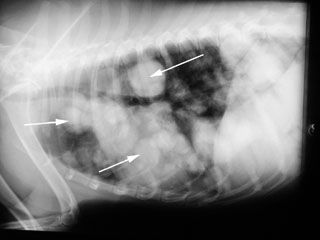 |
|
|
| Figure
23: This is a picture of tumors in the chest of a dog. These tumors
spread here from another location in the dog's body. The white arrows
identify only some of the masses. |
|