BUY THIS MANUAL NOW and have access to this article and 100's of others just like it!
View some of the 10+ Video clips found in the Equine Manual
foot | pastern and fetlock | canon bone regions | knee and upper front limb | hock | stifle and upper hind limb | neck region | different joints and locations | nutrition and supplements
Introduction:
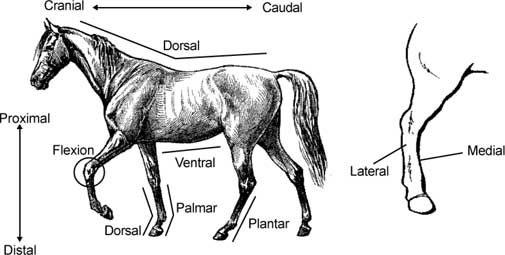
Today’s horse is a highly trained athlete that is often pushed to the very limits. Because of this, tendon, bone, hoof, and joint problems are some of the most common injuries many horse owners encounter. One of the keys to identifying and then treating these problems is understanding the terms and anatomical structures that may be involved. Another key is understanding the function of certain tendons, ligaments, and bones. To help understand these structures and their function, the pictures and captions on pages A28, A30, and A35 are essential. The following diagrams and definitions are also of benefit.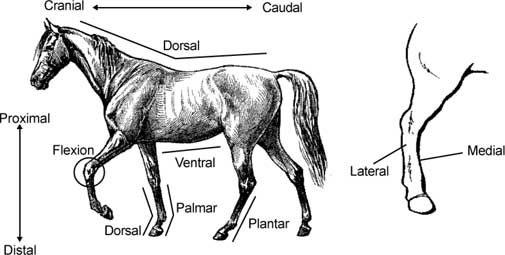
Terms:
Diagnosing a Problem:
Many times it is obvious that an injury has occurred. Other times the injury may be old, or the horse may not be showing significant signs of lameness. The suggestions, pictures, and information found on pages B885 and E460 can help a horse owner identify a lameness problem. The following information will identify the specific tendon, ligament, joint, bone, and foot problems that are common in horses. For the most part, the information will be broken down into sections based on anatomical location of where the problem is occurring. For example, all problems associated with fetlock will be discussed together in alphabetical order. A general category is found towards the end that contains problems that can be found in many different joints or locations. Details on the cause, clinical signs, diagnosis, and treatment of each problem will be included as needed. A brief discussion on the role of nutrition and supplements in bone and joint problems is also found at the end of the discussion.Note: The following reference has been used extensively to generate much of the information contained in this discussion: Ted S. Stashak, DVM, MS. Adams’ Lameness in Horses. Lea and Febiger, 1987.
BUY THIS MANUAL NOW and have access to this article and 100's of others just like it!
Figure 1
|
|
Treatment: The key to treating this problem is to bring the foot back
into balance by trimming the long heel. Some cases may resolve by simply
trimming and then letting the horse go bare foot. In other cases, the long heel
should be trimmed and a full bar shoe should be used to distribute the horse’s
weight evenly around the foot. With successive trimming and shoeing, the foot
can eventually come back into balance with both heels evenly on the ground
surface. In very severe cases, a normal return to function may not be
achieved.
Causative Agent: Sidebone is caused by concussion forces being placed
on the collateral cartilages. The collateral cartilages are found on either side
of the coffin bone of the foot and extend up past the coronary band. With
continued traumatic forces, the collateral cartilages begin to turn to bone (or
ossify). Sidebone is usually found in the front feet of horses that have
conformation problems. Animals that are base-narrow or base-wide have the
tendency to develop this problem.
Clinical Signs: Pain and heat are often noted over the collateral
cartilages during the active stages of the disease. The cartilages that are
involved will often be harder than normal and painful to the touch. These horses
may or may not be lame.
Diagnosis: It is often easy to falsely conclude that sidebone is the
cause for a horse’s lameness. Sidebone should not be diagnosed as the cause of
lameness unless there is heat and pain associated with the collateral
cartilages. Radiographs showing the cartilage turning into bone can be used to
identify this problem. This finding alone, however, is not sufficient to
diagnose sidebone without the associated signs of heat and pain.
Treatment: Some farriers recommend that the hoof wall over the
sidebone areas be thinned or grooved. These processes allow the foot to expand
and be more flexible. If fractures of the sidebone occur, they need to be
surgically removed. If pain and heat are still present, treating with
phenylbutazone can help. All cases should be rested until the inflammation has
subsided. In general, many cases are not lame and do not require treatment
unless there is active pain and heat.
Causative Agent: Thrush is caused by an infection of anaerobic bacteria and
potentially other organisms in the frog and sulcus (commissure). These organisms
infect horses that are kept
in moist, dirty environments, where the foot is continually dirty and wet. Feet
that are improperly shod or are improperly trimmed are also at risk of being
infected.
Clinical Signs: In most cases the commissures of the foot are full of a
dark, foul smelling discharge. The commissures are often deeper than normal, and
the frog can be loosened from the underlying tissues. In severe cases the
organisms can be infecting the sensitive structures of the foot causing lameness
and infections going up the limb.
Treatment: The treatment for thrush involves keeping the foot clean, dry,
and properly shod. After the foot is completely cleaned with a hoof pick and
knife, topical medications such as povidone-iodine (Betadine), chlorhexidine, or
Kopertox should be applied on a daily basis until the infection is cleared.
Causative Agent: Cracks can start from the bottom or the top of the hoof
wall and extend variable distances. The cracks that start at the coronary band
are usually caused by some type of trauma or injury to the coronary band. The
cracks that start at the bottom of the foot are most often caused by letting the
foot go too long without trimming. Excessive drying of the foot can also make it
more susceptible to cracking.
Clinical Signs: Depending on the severity of the cracks, some horses may
be lame. Some cracks may become infected and discharge blood or pus.
Treatment: The treatment for each crack will depend on its location,
depth, and how far up or down the hoof wall it extends. Any cracks with signs of
infection, should be treated with povidone-iodine (Betadine) and bandaged until
the infection is cleared. Current treatments for many cracks involves the use of
synthetic epoxy and hoof repair materials. Before these materials are placed in
the crack, the crack should be thoroughly cleaned and possibly burred out to
enlarge the area for the glue or plastic to adhere. Some horses should be shod
with toe clips placed on either side of the crack to prevent it from expanding (see figure
2).
Figure 2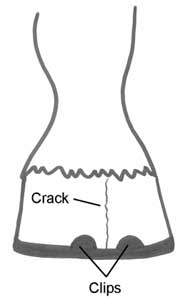
|
BUY THIS MANUAL NOW and have access to this article and 100's of others just like it!
Problems in the Pastern and Fetlock
| Figure 3: Mild windpuffs |
 |
Treatment: In many cases, resting the horse will help alleviate the
problem. In younger horses, the problem will often leave as the horse grows.
Pressure wraps and topical DMSO can be used if the problems persist.
Thorough-pin is the common term for tenosynovitis in the tarsal sheath that
surrounds the deep digital flexor tendon in the hind limb. This condition can be
identified by noting swelling of the tendon sheath above the fetlock on the back
of the hind limb. Thorough-pin is a mild form of tenosynovitis and should be
treated like a horse with windpuffs. Like windpuffs, the swelling in
thorough-pin is not hot, and the horse should not be painful or lame. Often the
cause of thorough-pin is not known.
BUY THIS MANUAL NOW and have access to this article and 100's of others just like it!
Problems in the Cannon Bone Regions (Metacarpus, Metatarsus, and Splint Bones)
| Figure 4: Splint |
 |
Diagnosis: Many cases can be identified by the clinical signs (location,
swelling, heat, and pain). If a fracture of the splint is involved, the swelling
and pain may be more extensive and severe. In some cases radiographs will need
to be taken to determine if a joint or the cannon bone is involved. If
interfering is suspected, place white chalk on the inside hoof of the opposite
limb. Work the horse and watch for evidence of chalk on the splint area.
Treatment: The treatment will vary depending on the cause; therefore, it
is important to determine the exact cause of the splints. For interfering
problems, using good splint boots will help resolve the problem. The idea behind
splint boots is to prevent the opposite limb from contacting the shin (cannon)
area. These boots contain some type of thickened material for protection. The
key to placing the boots is not necessarily how tight they are, but that they are placed properly to protect the shin
(cannon) bone areas. The horse should also be evaluated (by owner and farrier)
for any trimming or shoeing reasons for the horse to interfere. Most
conformation problems are difficult to correct. If nutrition in a young horse
might be the problem, use the information on page A575 to calculate what is
being fed. If the ration seems too hot, take measures to decrease the amount of
energy (TDN) being fed.
Anti-inflammatory agents (bute,
topical DMSO) and cold water soaks are essential for splints that are painful, tender, and
swollen. Cold water/ice can be applied
20 minutes twice a day for 5-7 days. After the soaks, pressure wrapping the
involved areas can also help. Rest is also essential until the inflammation has
gone down (30-45 days). If the splints are more chronic (have been going on for
some time), the above may not be useful. In these cases the extra bone may have
to be removed by surgery. In general, if the initial inflammation is reduced
early on, the outcome is usually favorable. It is also essential to remove the
cause (nutrition problems, interfering, etc.). Most splints resolve with time
and proper treatment.
Introduction and Causative Agent: All of these terms are used
to describe injury to the cannon bone that takes place when severe compression
forces are placed on the limb during impact. When bone remodeling cannot keep
up with the repeated stresses, defects in the bone occur. These injuries most
often occur in young animals (2-3 years of age) that are under extensive
training programs.
Clinical Signs and Diagnosis: In the acute, mild form of the disease,
the horse may be in pain when pressure is placed on the involved area of the
cannon bone. The horse is usually only sightly lame and the condition may even
go unnoticed. If the problem progresses, swelling may be felt on the
front/middle (dorsomedial) surface of the cannon bone. The pain is usually more
severe at this stage. In the early part of this problem, radiographs are often
normal. As the problem progresses, radiographs may show a subperiosteal callus
forming in the injured areas of the cannon bone. These calluses are the way the
bone tries to heal itself by laying down extra bone for added strength.
Occasionally, fractures are observed on a radiograph.
Treatment: For the more mild cases, rest and daily hand walking are
recommended. This should be continued until the cannon bone is no longer painful
to pressure. After this, the horse can be placed on a controlled exercise
program. The length and duration of the controlled exercise program is
determined by how well the cannon remains unpainful. Anti-inflammatory agents
are also of benefit. For the more severe cases, the extent of rest may go as
long as one year. There are some surgical procedures for those cases that do not
respond to rest and anti-inflammatory agents.
BUY THIS MANUAL NOW and have access to this article and 100's of others just like it!
Problems in the Knee (Carpus) and Upper Front Limb:
Problems in the Hock (Tarsus):
Clinical Signs: The excess joint fluid causes soft, fluid filled bulges to appear on the inside and outside areas of the hock (see figure 5). Like windpuffs, these swellings are not hot, and the horse should not be in pain or lame unless the bog spavin is due to an injury or OCD lesion. As pressure is placed on one of the swellings, the fluid will be pushed to other swellings and make them larger.
| Figure 5: Bog spavin |
 |
Diagnosis: It is important to determine the exact cause for the joint
swelling (OCD, trauma, nutrition, etc.). To do this a radiograph is a must.
Clinical Signs/Diagnosis: These horses
often have a history of being moderately lame after exercise, but improve with
rest. These horses are positive to the spavin or hock flexion test. To perform a
spavin test, the limb should be held in this position, with the cannon bone
parallel to the ground, for 1-2 minutes (see
figure 6). Once the limb is released, watch the horse for signs of lameness as
it is trotted away. Because of the inflammation to the periosteum (periostitis),
extra bone is formed over the front and inside areas of the hock joint. As a
result, a firm, boney bump can often be detected on the inside (medial) portion
of the lower hock (see figure 7). Radiographs are very important in diagnosing
this disease. Multiple views of both hocks are often necessary to help identify
the problem.
Video clip of a spavin test being performed. If the video
does not play, you must install an MPEG video
Treatment: In many cases of bone spavin, treatment efforts are not very
effective. Many horses remain lame and never return to full function. There are
various surgical techniques that can be used to help treat bone spavin. The most
common is a procedure called a cunean tenectomy. This procedure removes the
portion of the cunean tendon where it moves over this region of the hock.
Corrective shoeing can also help many of these horses. The intent of the
corrective shoeing should be to cause the foot to break-over quicker. This can
be accomplished by using a rocker or rolled toed shoe.
Clinical Signs and Diagnosis: Signs of heat, swelling, pain, and lameness
are common early on in the condition. As things progress, scar tissue and an
obvious bump may be noticed (see figure 8). Radiographs can help determine the
cause and extent of a suspected case of curb.
Treatment: In many cases, resting the horse will help alleviate the
problem. Rest should be accompanied by ice packs, anti-inflammatory agents, and
corticosteroid injections under the skin in the area of the lesion. In cases
that have been going on for sometime, successful treatment may not be
achieved.
BUY THIS MANUAL NOW and have access to this article and 100's of others just
like it! Problems in the Stifle and Upper Hind Limb
Treatment: In many cases, resting the horse will help alleviate the
problem. In younger horses, the problem will often leave as the horse grows. If
the problem is due to OCD, surgical treatment of the lesion is necessary. When
nutritional deficiencies are the cause, supplementation is required. If the
problem is severe or the horse is lame and painful, injections of
corticosteroids and other products may be given in the joint. Some of the
anti-inflammatory and glycosaminoglycan products may also be of benefit. Because
no treatment seems to be 100% effective, bog spavin is sometimes a difficult
problem to completely cure. This is particularly true if the problem is caused
by a conformation defect or trauma.
Introduction and Causative Agents: Bone spavin is found most often in
horses that are ridden at high speeds, where they are used for jumping, reining,
roping, and cutting. Damage and inflammation occurs in the lower bones and
joints of the hock when compression and rotation stresses are placed on the hock
during these exercises. Like bog spavin, these injuries are often the result of
poor conformation (straight, cow, or sickle hocked). Some studies show that
nutritional imbalances and deficiencies may also play a role in this disease.
Figure 6: Spavin test

player on your computer (e.g. Windows Media Player).
Click here to
download Windows Media Player.
Or
Install Internet Explorer from our CD Manual.
Figure 7: Bone spavin

Introduction and Causative Agents: Curb is a condition where the back
(plantar) aspect of the fibular tarsal bone is enlarged. This results from an
enlargement of the plantar ligament due to inflammation and thickening. In some
cases periostitis is involved and there is an extra layer of bone in that
region. The plantar ligament is located in the area just below the point of the
hock. Inflammation of the plantar ligament is often the result of poor
conformation (straight, cow, or sickle hocked) or when the horse injures itself
in the hock region by kicking against trailers or walls.
Figure 8: Curb
Introduction: The patella is the horse’s knee cap. It can be
fractured, luxated, or become fixated or "stuck."
Causative Agents: Luxations and fractures are due to trauma caused by
kicks and collisions. Luxations can also be due to congenital abnormalities. The
upward fixation of the patella is caused by genetic traits where the horse has a
"straight hind limb" conformation. Poor muscling and muscle tone can
also be part of the problem. In this situation, the patella becomes fixed or
catches on a ridge (medial trochlear ridge) of the femur. This prevents the limb
from flexing.
Clinical Signs and Diagnosis: When luxations and fractures are the
problem, the stifle will be swollen and painful. The horse may show varying
degrees of lameness. Radiographs are also helpful in diagnosing these problems.
If the horse has a problem with upward fixation of the patella, the limb may
actually be "locked" in a flexed position where the stifle and hock
cannot flex. If the horse is only "catching" the patella on the ridge,
the horse will have a jerky gait when turned in a circle or walked up or down a
hill.
Treatment: For luxations and fractures, surgical procedures can be
used to help treat the problem. For minor fractures, stall rest and splints may
be all that is needed. Treatment for a fixed patella depends on how severe it is
and if the patella is "locked" or just "catches." For
immediate treatment of a locked patella, the limb can be pulled forward, while
pressure is placed on the patella to force it down and medially. The horse can
also be backed down a hill, while the same pressure is placed on the patella to
force it down and medially. Some recommend startling the horse, causing the
patella to release. This should be done with caution because of the potential
for additional injury. In the more severe cases, surgery can be performed to cut
the medial patellar ligament. This allows the patella to release and prevents
any additional locking of the patella on the medial trochlear ridge of the
femur. Once the surgery is performed, the horse should not be used for at least
6 weeks.
Prognosis: For luxations, the prognosis is guarded to poor. For fractures
of the patella, the prognosis can be favorable if proper and thorough treatment
is implemented. The prognosis for upward fixation of the patella is good as long
as the joint has not suffered any permanent damage.
The following video clip shows a pony with a fixated
patella in the left hind limb. The patella remains fixated throughout
the entire video.
|
If the video
does not play, you must install an MPEG video |
BUY THIS MANUAL NOW and have access to this article and 100's of others just
like it! Problems in the Neck Region
Introduction: Fractures of the tibia, femur, and pelvis will be
discussed below. In general, fractures that occur in foals have a greater
chance of being treatable. Direct injury or trauma to the area is usually the
cause of these fractures. This injury can come from a kick, severe compression
forces, or accident (collision). The resulting injury can be anything from a
fissure fracture to a comminuted (multiple pieces) fracture.
Clinical Signs and Diagnosis: Non-weight bearing lameness is often
noted with these fractures. In most cases, swelling, pain, and crepitus
("grinding") can be found when the area is handled and manipulated.
Diagnosing these injuries is not usually difficult and radiographs are the best
way to determine the extent and type of fracture.
Treatment and Prognosis: In general, most significant fractures in the
tibia or femur of an adult horse are difficult to treat. Many of these horses
should be euthanized. This statement is also true for many fractures of the
femur in a foal. On the other hand, some minor fractures of the tibia can be
treated with only strict stall rest. The more complicated fractures of the tibia
and femur in a foal can sometimes be treated with surgery and/or cast
application. During the surgery, plates, screws, and pins may be used to hold
the fracture in place. There is no surgical treatment for fractures of the
pelvis. A fractured pelvis may be treated with strict stall rest for as long one
year. Slings may also be used for the first 6-8 weeks. Because there is such
variability in the types and treatments of these fractures, a veterinarian must
be involved in each individual case.
Again, no matter what type of fracture has
occurred, attention should be given to the opposite limb. In many cases, the
opposite limb will be forced to bear most of the weight. This can result in
laminitis and other problems.
Some foals with these types of fractures
do fairly well after successful treatment. If the horse is a yearling or adult,
the fracture has broken the skin, or the fracture is comminuted, the prognosis
is poor.
Introduction: The term "wobblers" is often used to describe
any condition of the horse where weakness and coordination problems are
involved. This condition can be caused by deformed vertebrae in the neck
(cervical vertebral malformations), equine protozoal myeloencephalitis
(EPM),
equine herpes, equine infectious anemia, trauma, and others. This discussion
will describe wobbler syndrome caused by deformed vertebrae in the neck. The
other conditions have been discussed elsewhere in this manual.
Causative Agent: Wobbler syndrome is caused by a defect in the
vertebrae of the neck that compresses the spinal cord. The deformed vertebrae
can compress the spinal cord all the time or only when the neck is flexed.
Studies indicate that this condition has some genetic and nutritional influences
that cause the vertebrae to not form properly. Horses that are fed high energy
diets, grow rapidly, and are large at a young age are more at risk.
Clinical Signs: Ataxia (balance problems), gait abnormalities, and
weakness are some of the common signs. Many horses are in pain and reluctant to
move their necks. Some horses recover and remain fairly normal, while others
digress to an unmanageable state.
Diagnosis: A physical exam will help to identify the possible location of
the problem. Radiographs are essential to determine exactly where the problems
are located and the severity of the deformities. These examinations may also
reveal degenerative joint disease (DJD) and osteochondritis dissecans (OCD)
lesions.
Treatment and Prognosis: Some mild cases may respond to anti-inflammatory
agents (steroids, bute) that help to reduce the inflammation in the spinal cord
and surrounding areas. This type of treatment only produces temporary
improvement, with the horse continuing to have problems. In most cases the
surgical treatment is a must. The surgical procedures that are commonly used are
designed to provide increased stability to the neck vertebrae. Most surgical
cases can return to breeding and a few horses may return to normal or near
normal function. Horses that show few clinical signs prior to surgery, have a
better chance of gaining a favorable recovery.
Problems Found in Many Different Joints and Locations
When abnormal amounts of
weight and pressure are placed on a growth plate or area of endochondral
ossification, the growth is stunted. For example, one way to cause a carpus
valgus deformity in a foal is to have an injury or poor conformation that causes
abnormal weight to be placed on the outside regions (lateral aspect) of the bone
(radius) above the knee (carpus) in the front limb. In this case, the outside
portion of the growth plate will NOT grow properly, while the inside (medial
aspect) will continue to grow. This causes the bone (radius) to cup or dish,
forcing the knees together. Nutritional imbalances, injury, and improper weight
bearing can also cause the growth plate to become inflamed (physitis) or even
close prematurely. This can result in abnormal growth and angular limb
deformities.
Clinical Signs: In severe cases, it is obvious that there is a problem
just by looking at the limbs. The horse may be lame and have swollen and painful
joints or growth plates.
Diagnosis: Radiographs are essential in identifying the location and
severity of the problem. A complete history should be taken and include the
following questions: Was the foal born this way? What is the diet? Was the mare
overweight during the pregnancy? Have there been any injuries to the limbs or
limb? A diagnosis can be reached based on the history, physical exam, and
radiographs.
Treatment: Treatment in all cases varies according to the cause of the
deformity. In general, there are three common avenues of treatment:
In general, if the problem is corrected early, most young foals have a
successful outcome.
Introduction: Flexural limb deformities are situations where the
various joints of the body are held in some degree of flexion. This is most
often the result of a contracted tendon. These problems are identified as
congenital (present at birth) or acquired (occurring after birth).
Causative Agents: Congenital deformities are most often caused
by malposition during the pregnancy, the mare ingesting toxic substances, and/or
inherited genetic defects. Acquired defects are often the result of pain
(epiphysitis, osteochondrosis, injury), genetics, nutritional imbalances
(excessive energy intake), and rapid growth. A combination of two or more of
these problems may also be the cause in some cases.
Clinical Signs and Diagnosis: In many cases more than one limb is
involved. Most of the time the knee (carpus) or fetlock is involved, and these
joints are often "popped" forward. The joint is held in this flexed
position, and may or may not be forced to a normal position with pressure. The
acquired cases will often result in a "club foot," where the horse
bears its weight on the toe.
Treatment for Congenital Deformities: Some horses will correct the
problem on their own with little or no human intervention. More complicated
cases can be helped/treated in one of three ways:
| Figure 9: Carpal hygroma |
 |
Clinical Signs: Some pain, heat, and swelling are the most common signs.
If the injury is significant, the swelling can be quite large and there can be
some soft tissue thickening.
Treatment: In most cases, the bursitis can be treated with ice packs,
anti-inflammatory agents, and rest. It is also important to prevent additional
injury to the bursa (remove the shoe on that foot, etc.). For more severe cases,
injections into the problem area and surgery may be required.
Introduction: "Epiphysitis" is a problem that is commonly
found in young, growing animals (ages 4-8 months) and young horses beginning
training. The term "Epiphysitis" is somewhat misleading because the
problem actually involves the growth plate and not the end (epiphysis) of a long
bone.
Causative Agents: Fast growing, young animals that are fed high grain
rations seem to have the most problems. Genetics may also play a role in the
fact that faster growing foals experience epiphysitis. Abnormal weight bearing
and trauma/injury to the growth plate are sometimes associated with this
disease. Studies indicate that a combination of these influences is often the
cause. With the above being the known causes for epiphysitis, how they actually
cause the disease is less understood.
Clinical Signs: The most obvious sign is a "flaring" or
enlargement of the ends of the long bones. This commonly is seen above the knees
on the end of the radius. As the problem progresses, the end of the bone begins
to take on a "hour glass" shape. Depending on the severity of the
disease, the horse may or may not be lame. The horse may act painful when the
involved area is palpated or handled.
Diagnosis: Physical exam and radiographic images are often sufficient
to diagnose this problem.
Treatment and Prevention: The most important step in treating and
preventing this disease is to evaluate and adjust the horse’s ration. Any
nutritional imbalances should be corrected. Use the information found on page
A575 and the details contained below on nutrition to help calculate a proper
diet. Mineral analysis may need to be performed to determine any deficiencies or
excesses of the trace minerals. If the horse is over weight, restrict the amount
of energy being fed. Some horses may recover with rest and the proper use of
anti-inflammatory agents (bute). If anti-inflammatory agents are used, the foal will use the limb
more as the pain and inflammation is reduced.
This potentially can result in additional injury and epiphysitis. If radiographs show that
there are other problems (OCD lesions, angular limb deformities), these will
need to be corrected to help alleviate the epiphysitis. Many horses seem to
recover with time and rest; however, they never return to full performance
ability.
Introduction and Causative Agents: A luxation is a dislocation of a
joint and can occur in the fetlock, knee (carpus), shoulder, hock (tarsus),
stifle, and hip. These injuries most often occur when the limb is forced in an
abnormal direction. This can happen when the horse steps in a hole, falls,
slips, jumps, or twists the limb while in a flexed or extended position.
Clinical Signs: The limb that is involved often has a angular
deformity, where the portion of the limb distal to luxated joint is deviated
outward or inward. The joint itself maybe swollen, painful, and unstable. There
will also be varying degrees of lameness.
Diagnosis: Diagnosing the location of these injuries is not usually
difficult. Radiographs are the best way to confirm a diagnosis and determine if
any fractures are involved.
Treatment: Treatment for most luxations requires that the horse be
anesthetized and the dislocation be reduced or put back into place. This should
take place as soon as possible after the injury. Depending on the location of
the luxation, casts may also be applied. Any chip or other type of fracture
should be treated appropriately.
Prognosis: Many of the minor luxations where no fractures are involved
will often have a good recovery and return to performance. Luxations of the hip
joint, however, may never return to normal even after the head of the femur is
put back into place. If fractures, infection, or degenerative joint disease (DJD)
occur, the prognosis is poor.
Introduction: Osteochondrosis is a defect in the normal development of
cartilage. This defect occurs sometime in the process of endochondral
ossification. Endochondral ossification is where cartilage (in the epiphysis or
ends of the long bones) actually ossifies to form bone. If endochondral
ossification does not progress normally, defects called osteochondritis
dissecans (OCD) or subchondral bone cysts can result. OCD lesions are places
where fragments or flaps of cartilage associated with the joint are separated
from the rest of the cartilage. Bone cysts are areas in the end of the bone
where endochondral ossification does not progress normally. This leaves small
areas of cartilage deep within the end of the bone. These areas necrose or die
and leave a defect in the end of the bone.
Causative Agents: The following are thought to cause these defects in
a growing animal:
Causative Agents and Clinical Signs: In most cases, these problems are
caused by severe straining and over-stretching of the tendon or ligament. This
can occur when excessive loads are placed on the limbs due to sudden turns,
jumping, stopping, or slipping. Things such as improper shoeing, poor
conformation, and traumatic injuries can also cause a problem to develop. When
injury occurs to the tendon, the tendon fibers can be damaged and the blood
supply can be compromised. Severe injury can result in complete rupture of the
tendon.
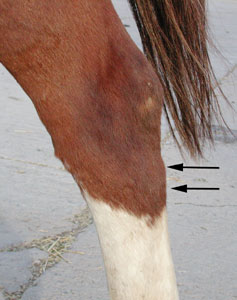
Clinical Signs: After the initial injury, the involved area is swollen,
painful, and hot to the touch. The horse is often lame and very painful when the
limb is flexed. These injuries can occur in the flexor tendons located behind
the cannon bone ("bowed tendon") in the area just below the knee or hock and
above the fetlock (see figure 10). In some cases it is an injury to the anular
ligament that causes the problem. The anular ligament wraps itself around the
fetlock area (kind of like shrink wrap) and helps to keep all the tendons and
joint structures encapsulated. If the anular ligament becomes inflamed, it may
begin to scar and shrink. The superficial flexor tendon runs just beneath this
anular ligament. If the anular ligament scars and constricts, the flexor tendon
is "pinched." This can be the cause of the swelling above a fetlock
joint. If these problems continue for prolonged periods of time, the tendon can
begin to scar and adhere to surrounding tissues. This will cause a loss of
function and flexibility of the tendon/ligament. In some cases the navicular and
sesamoid bones may be involved. If the sesamoids are inflamed, it is called
sesamoiditis.
| Figure 10: Bowed tendon |
 |
BUY THIS MANUAL NOW and have access to this article and 100's of others just
like it! Nutrition and Supplements: Proper nutrition plays an essential role in the development of healthy bones,
muscles, and related structures. Consuming rations that contain imbalances in
protein, minerals, and vitamins can cause abnormal bone development. Too much
feed intake can be as detrimental as too little feed intake. Because most of the
nutrition related problems occur in foals, attention should be given to the
ration being fed to a pregnant/lactating mare. In general, if the mare does not
consume sufficient amounts of a properly balanced diet, overall milk production
will be low, and the milk will lack the essential vitamins and minerals
(calcium, phosphorus, vitamin A, copper) necessary for a healthy foal. If the
mare consumes too much high quality feed, she will be overweight and still not
produce sufficient quantities of milk for the foal because of excess fat
deposits in the mammary gland. An overweight mare will also not breed back as
well. Pregnant mares and ones that are lactating should be feed a diet that is at
least 12-14% protein on a dry matter basis. Their milk should contain 80-120
mg/dl of calcium and 45-90 mg/dl of phosphorus. They should be fed a balanced
ration that contains vitamin A, copper, zinc, and possibly manganese. Because
the mare’s ability to produce sufficient quantities of milk declines with
time, it is important to begin creep feeding foals at a young age (3-4 weeks).
Remember, however, that feeding foals excess protein (greater than 2% of the
foals requirement), zinc, selenium, and iodized salt, can result in bone, hoof,
and hair problems. Additional information on creep feeding and nutrition can be
found on pages A249 and A575. In many cases, the use of dietary supplements is not necessary and can even
be detrimental to the horse. This statement is true only if the horse has access
to sufficient amounts of a balanced diet. Supplements should be used when a
deficiency in the diet is present, a specific joint disease is diagnosed, or
when the horse has the potential to develop a joint, muscle, or tendon problem. To fully understand the common supplements that are used to maintain healthy
joints, it is important to know something about what makes a healthy joint. Many
of the joints in the body (knee, hock, fetlock, etc.) contain cartilage and
synovial or joint fluid. These joints are surrounded by a synovial membrane and joint
capsule. Healthy cartilage and synovial fluid are essential in order to provide
a low friction, smooth surface for the bones of the joint to move against and
impact with. Realize that stresses placed on the joint during training and
competition cause wear and tear to the joint cartilage and inflammation. If
damage is severe or the inflammation continues for extended periods of time, the
cartilage and joint can be permanently injured. Articular cartilage has the ability to replenish itself when mild damage
occurs. It does this by producing collagen and proteoglycans. Collagen is a
protein that provides the strength of cartilage, while proteoglycans (made of
glycosaminoglycans) provide resistance to compressive forces. Most of the joint
supplements contain raw materials or nutrients that are required to allow the
cartilage to replenish itself and ingredients that help reduce inflammation in
the joint. Glucosamine HCI, chondroitin sulfate, and methylsulfonylmethane (MSM)
are some of these ingredients. Glucosamine is required for the production of
glycosaminoglycans and proteoglycans. It also helps reduce
inflammation. Chondroitin sulfate is one of the major glycosaminoglycans found
in cartilage and also helps to reduce inflammation. Methylsulfonylmethane (MSM)
acts as an anti-inflammatory and general pain reliever. The following list identifies some common joint/muscle/tendon supplements
that can be useful in many horses: The following are products that can be injected or given orally to help
relieve joint inflammation and pain: Summary: In conclusion, joint, bone, tendon, and ligament injuries can
often be challenging problems to diagnose and resolve. If a problem does not
improve with routine treatments, be sure to involve a local veterinarian.
BUY THIS MANUAL NOW and have access to this article and 100's of others just
like it!
View More of the 10+
Video clips found in the Equine
Manual
Diagnosis: Many cases are identified based on physical exam and
clinical signs. The severity of the problem can often be determined through the
use of ultrasound and radiography.
Treatment: The key to healing acute tendon/ligament problems is to reduce
the inflammation and keep any additional trauma and swelling from occurring.
Treatments to reduce the inflammation include cold water soaks or ice packs for
20 minutes twice a day for the first 2-3 days and anti-inflammatory agents (bute).
Topical DMSO can also be beneficial in reducing the swelling. Pressure wraps and
even casting can be used in more severe cases to prevent additional stretching
and injury to any of the tendons and ligaments. To prevent additional injury,
strict stall rest (for the first two weeks), followed by mild manipulations of
the injured area, should be used. To help build the tendon, regularly pick up the
foot/leg and move it gently through a series of flexing motions.
Excessive flexion, particularly where the horse shows pain, will cause continued
damage and should be avoided.
After the rest and mild manipulations, carefully choose what activities the
horse is asked to perform. These should be low impact and preferably without a
rider. Some minor tendon stretching will occur with normal use. After
these occasions, reduce the chance for inflammation and swelling by using cold
water soaks and anti-inflammatory agents as needed. If continued irritation
occurs, scaring and permanent injury will result.
For the more chronic tendon/ligament injuries, where scarring and boney damage
may be involved, surgical intervention is often required. There are many
different procedures that can be used. An equine surgeon will need to evaluate
each situation before a recommendation can be given. The usual treatment for
bowed tendons caused by anular ligament problems is a surgical procedure where
the anular ligament is cut. This allows the flexor tendons to move more freely.